J Korean Surg Soc.
2011 May;80(5):319-326. 10.4174/jkss.2011.80.5.319.
Laparoscopic totally extraperitoneal repair without suprapubic port: comparison with conventional totally extraperitoneal repair
- Affiliations
-
- 1Department of Surgery, Kangbuk Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. byunghomd.son@samsung.com
- KMID: 2212156
- DOI: http://doi.org/10.4174/jkss.2011.80.5.319
Abstract
- PURPOSE
We have treated 24 patients through laparoscopic totally extraperitoneal (TEP) repair without suprapubic port by using reliability and reducing the invasiveness of two surgery. This study is aimed to assess the safety and feasibility of the TEP repair without suprapubic port compared to conventional TEP repair.
METHODS
From September 2007 to 11 May 2010, we compared two groups that suffer from inguinal hernias. One is comprised of 24 patients who were treated without suprapubic port laparoscopic totally extraperitoneal repair (Group A), and the other is comprised of 100 patients who were treated with conventional laparoscopic totally extraperitoneal repair (Group B). Data regarding patient demographics (sex, age, site of hernia, and the type of hernia), operating time, postoperative hospital stay, the use of analgesics, and complications were prospectively collected.
RESULTS
There was no significant difference noted between two groups in relation to sex, age, site, and the type of hernia. The mean operating time and postoperative hospital stay was longer for the Group B (62.9 minutes, 3.55 days) than for the Group A (59.0 minutes, 2.54 days) (P = 0.389, P < 0.001). Postoperative urinary retention, seroma, wound infection were respectively 4.2%, 8.3%, 0% in Group A, and 12.0%, 8.0%, 7% in group B. There was difference between the two groups, but not statistical significance. Group B used more analgesics than Group A (0.33 vs. 0.48), but it wasn't significant statistically (P = 0.234).
CONCLUSION
Although prospective randomized studies with long-term follow-up evaluation are needed to confirm our study between laparoscopic totally extraperitoneal repair without suprapubic-port and conventional laparoscopic totally extraperitoneal repair, our method have some advantages in postoperative pain, urinary retention, operating time, postoperative hospital stay, and cosmetic effect.
MeSH Terms
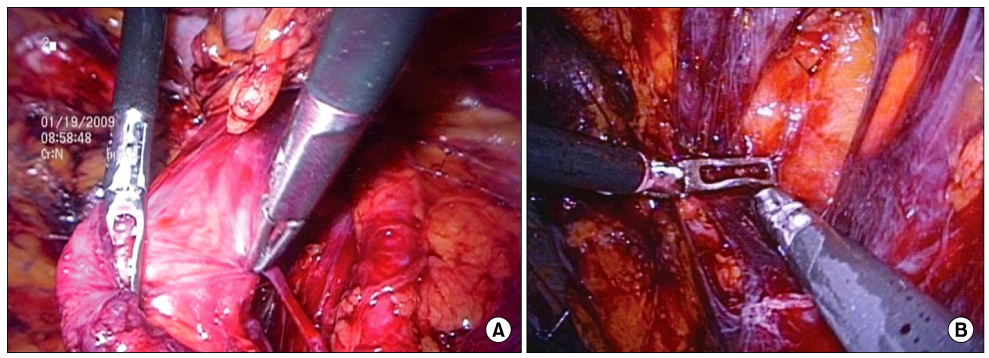
Figure
Reference
-
1. Bassini E. Nuovo metodo per la cura radicale dell'ernia inguinale. Atti Congr Assoc Med Ital. 1887. 2:179.2. Kumar S, Wilson RG, Nixon SJ, Macintyre IM. Chronic pain after laparoscopic and open mesh repair of groin hernia. Br J Surg. 2002. 89:1476–1479.3. Memon MA, Cooper NJ, Memon B, Memon MI, Abrams KR. Meta-analysis of randomized clinical trials comparing open and laparoscopic inguinal hernia repair. Br J Surg. 2003. 90:1479–1492.4. Heikkinen TJ, Haukipuro K, Koivukangas P, Hulkko A. A prospective randomized outcome and cost comparison of totally extraperitoneal endoscopic hernioplasty versus Lichtenstein hernia operation among employed patients. Surg Laparosc Endosc. 1998. 8:338–344.5. Liem MS, van der Graaf Y, van Steensel CJ, Boelhouwer RU, Clevers GJ, Meijer WS, et al. Comparison of conventional anterior surgery and laparoscopic surgery for inguinal-hernia repair. N Engl J Med. 1997. 336:1541–1547.6. Johansson B, Hallerbäck B, Glise H, Anesten B, Smedberg S, Román J. Laparoscopic mesh versus open preperitoneal mesh versus conventional technique for inguinal hernia repair: a randomized multicenter trial (SCUR Hernia Repair Study). Ann Surg. 1999. 230:225–231.7. Surgit O. Single-incision laparoscopic surgery for total extraperitoneal repair of inguinal hernias in 23 patients. Surg Laparosc Endosc Percutan Tech. 2010. 20:114–118.8. He K, Chen H, Ding R, Hua R, Yao Q. Single incision laparoscopic totally extraperitoneal inguinal hernia repair. Hernia. 2010. 05. 14. [Epub]. DOI: 10.1007/s10029-010-0674-z.9. Agrawal S, Shaw A, Soon Y. Single-port laparoscopic totally extraperitoneal inguinal hernia repair with the TriPort system: initial experience. Surg Endosc. 2010. 24:952–956.10. Koch CA, Grinberg GG, Farley DR. Incidence and risk factors for urinary retention after endoscopic hernia repair. Am J Surg. 2006. 191:381–385.11. Winslow ER, Quasebarth M, Brunt LM. Perioperative outcomes and complications of open vs laparoscopic extraperitoneal inguinal hernia repair in a mature surgical practice. Surg Endosc. 2004. 18:221–227.12. Classification of chronic pain. Descriptions of chronic painsyndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl. 1986. 3:S1–S226.13. Nyhus LM, Codon RE. Hernia. 1995. 4th ed. Philadelphia: JB Lippincott;3–199.14. Lichtenstein IL, Shore JM. Simplified repair of femoral and recurrent inguinal hernias by a "plug" technic. Am J Surg. 1974. 128:439–444.15. Ger R, Mishrick A, Hurwitz J, Romero C, Oddsen R. Management of groin hernias by laparoscopy. World J Surg. 1993. 17:46–50.16. Hawasli A. Laparoscopic inguinal herniorrhaphy: the mushroom plug repair. Surg Laparosc Endosc. 1992. 2:111–116.17. Arregui ME, Davis CJ, Yucel O, Nagan RF. Laparoscopic mesh repair of inguinal hernia using a preperitoneal approach: a preliminary report. Surg Laparosc Endosc. 1992. 2:53–58.18. McKernan JB, Laws HL. Laparoscopic repair of inguinal hernias using a totally extraperitoneal prosthetic approach. Surg Endosc. 1993. 7:26–28.19. Youn SI, Kim BG, Cha SJ, Chang IT. The comparative analysis between laparoscopic inguinal herniorrhaphy and open inguinal herniorrhaphy. J Korean Surg Soc. 2005. 69:166–171.20. EU Hernia Trialists Collaboration. Laparoscopic compared with open methods of groin hernia repair: systematic review of randomized controlled trials. Br J Surg. 2000. 87:860–867.21. Juul P, Christensen K. Randomized clinical trial of laparoscopic versus open inguinal hernia repair. Br J Surg. 1999. 86:316–319.22. Esposito C. One-trocar appendectomy in pediatric surgery. Surg Endosc. 1998. 12:177–178.23. Piskun G, Rajpal S. Transumbilical laparoscopic cholecystectomy utilizes no incisions outside the umbilicus. J Laparoendosc Adv Surg Tech A. 1999. 9:361–364.24. Bailey HR, Ferguson JA. Prevention of urinary retention by fluid restriction following anorectal operations. Dis Colon Rectum. 1976. 19:250–252.25. Beadnell SW, Connaughton B, Farhood VW. Management of postoperative urinary retention. J Oral Maxillofac Surg. 1989. 47:1307–1310.26. Ferzli G, Sayad P, Huie F, Hallak A, Usal H. Endoscopic extraperitoneal herniorrhaphy. A 5-year experience. Surg Endosc. 1998. 12:1311–1313.27. Vidović D, Kirac I, Glavan E, Filipović-Cugura J, Ledinsky M, Bekavac-Beslin M. Laparoscopic totally extraperitoneal hernia repair versus open Lichtenstein hernia repair: results and complications. J Laparoendosc Adv Surg Tech A. 2007. 17:585–590.28. Koch CA, Grinberg GG, Farley DR. Incidence and risk factors for urinary retention after endoscopic hernia repair. Am J Surg. 2006. 191:381–385.29. Kulaçoğlu H, Dener C, Kama NA. Urinary retention after elective cholecystectomy. Am J Surg. 2001. 182:226–229.30. Han MS, Lee SM, Choi SI, Joo SH, Hong SW. Comparison of laparoscopic totally extraperitoneal inguinal hernia repair and tension-free herniorrhaphy using perfix (R): short-term follow-up results. J Korean Surg Soc. 2009. 77:189–194.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Totally Extraperitoneal Laparoscopic Repair of Obturator Hernia withPartial Intestinal Obstruction
- Prevention and management of intraoperative complication during single incision laparoscopic totally extraperitoneal repair
- SUTI (Single Umbilical Tangential Incision) Laparoscopic TEP Inguinal Hernia Repair
- To Minimize Post-operative Pain in Inguinal Hernia Repair: Single-port Laparoscopic Totally Extraperitoneal Inguinal Hernia Repair without Fixation of the Mesh
- Is a Single Incisional Laparoscopic Totally Extraperitoneal Approach Feasible for Inguinal Hernia Repair?