J Periodontal Implant Sci.
2013 Oct;43(5):243-247. 10.5051/jpis.2013.43.5.243.
Segmental osteotomy for mobilization of dental implant
- Affiliations
-
- 1Department of Oral Implantology, Dental School, Universidad de La Frontera, Temuco, Chile. sergio.olate@ufrontera.cl
- 2Department of Oral and Maxillofacial Surgery, Dental School, Universidad de La Frontera, Temuco, Chile.
- KMID: 2212034
- DOI: http://doi.org/10.5051/jpis.2013.43.5.243
Abstract
- PURPOSE
The aim of this work is to evaluate a surgical technique for mobilization of mal posed dental implant in anterior area.
METHODS
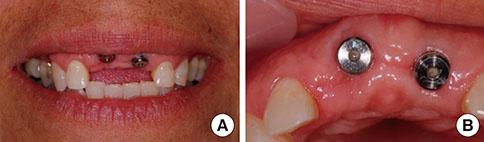
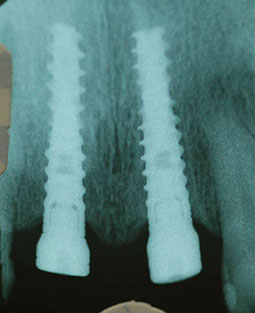
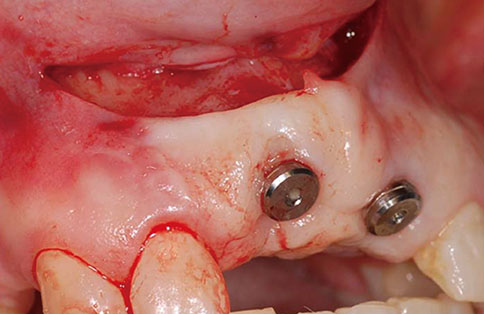
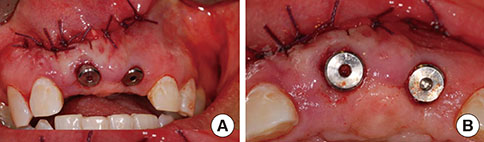
A 38-year-old patient consulted our unit for esthetic dissatisfaction with the implant treatment of a central incisor. An implant was observed in 11 and 21, where 11 was 3 mm above the ideal limit, with excessive vestibular angulation. The choice was made to perform a segmental osteotomy and mobilize the bone block and the implant down and forward; a bone block extracted from the mandibular ramus was installed between the implant block and the bed to stabilize the segment.
RESULTS
After 4 months, a conventional fixed prosthesis was created and the esthetic result achieved was close to what the patient wanted, with no need for further surgery. The surgical condition was stabilized and maintained for the long-time and no complications how necrosis, infection or bone defects was present.
CONCLUSIONS
It was concluded that the procedure is efficient, and the biological arguments in favor of the procedure are discussed.
Keyword
MeSH Terms
Figure
Reference
-
1. Scacchi M. The development of the ITI dental implant system Part 1: a review of the literature. Clin Oral Implants Res. 2000; 11:Suppl 1. 8–21.2. Scacchi M, Merz BR, Schar AR. The development of the ITI dental implant system. Part 2: 1998-2000: steps into the next millennium. Clin Oral Implants Res. 2000; 11:Suppl 1. 22–32.3. Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004; 19:Suppl. 43–61.4. Higginbottom F, Belser U, Jones JD, Keith SE. Prosthetic management of implants in the esthetic zone. Int J Oral Maxillofac Implants. 2004; 19:Suppl. 62–72.5. Grunder U, Gracis S, Capelli M. Influence of the 3-D bone-to-implant relationship on esthetics. Int J Periodontics Restorative Dent. 2005; 25:113–119.6. Zechner W, Bernhart T, Zauza K, Celar A, Watzek G. Multidimensional osteodistraction for correction of implant malposition in edentulous segments. Clin Oral Implants Res. 2001; 12:531–538.
Article7. Kassolis JD, Baer ML, Reynolds MA. The segmental osteotomy in the management of malposed implants: a case report and literature review. J Periodontol. 2003; 74:529–536.
Article8. Olate S, Kluppel LE, de Miranda Chaves Netto HD, Stabile GA, Mazzonetto R, de Albergaria-Barbosa JR. Sitios donantes mandibulares en implantología: Una evaluación clínica. Int J Odontostomatol. 2007; 1:121–127.9. Bell WH, You ZH, Finn RA, Fields RT. Wound healing after multisegmental Le Fort I osteotomy and transection of the descending palatine vessels. J Oral Maxillofac Surg. 1995; 53:1425–1433.
Article10. Mazzonetto R, Allais M, Maurette PE, Moreira RW. A retrospective study of the potential complications during alveolar distraction osteogenesis in 55 patients. Int J Oral Maxillofac Surg. 2007; 36:6–10.
Article11. Puleo DA, Thomas MV. Implant surfaces. Dent Clin North Am. 2006; 50:323–338.
Article12. Martin RJ, Goupil MT, Goldschmidt M. Single-implant segmental osteotomy: a case report. Int J Oral Maxillofac Implants. 1998; 13:710–712.13. Raghoebar GM, Visser A, Vissink A. Correction of a malpositioned endosseous implant by a segmental osteotomy: a case report. Int J Oral Maxillofac Implants. 2005; 20:627–631.14. Kao SY, Fong JH, Chou SJ, Wu JH, Tu HF, Yeung TC. Segmental osteotomy to reposition multiple osseointegrated dental implants in the anterior maxilla in a trauma patient. Dent Traumatol. 2007; 23:56–59.
Article15. Netto HD, Olate S, Mazzonetto R. Surgical repositioning of osseointegrated malposed dental implant with segmental osteotomy. J Craniofac Surg. 2012; 23:1540–1542.
Article16. Adolfi D, de Freitas AJ, Groisman M. Achieving aesthetic success with an immediate-function implant and customized abutment and coping. Pract Proced Aesthet Dent. 2005; 17:649–654.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Oral rehabilitation with mandibular anterior segmental osteotomy and implantation: A case report
- Office-based 2-stage Posterior Maxillary Segmental Osteotomy for Mandibular Implant Placement: Clinical Study
- Interdisciplinary Approaches for Resolution of Non-Ideal Interocclusal Space Prior to Dental Implant Treatments
- Minimum Presurgical Orthodontic Treatment with Two Jaw Surgery Combined with Anterior Segmental Osteotmy in Skeletal Class II Malocclusion: A Case Report
- Evaluation of soft tissue change after segmental osteotomy in Korean