J Korean Surg Soc.
2010 May;78(5):314-319. 10.4174/jkss.2010.78.5.314.
Comparison of Outcomes between Primary Closure vs. Patch Angioplasty in Carotid Endarterectomy
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. dikim@skku.edu
- 2Department of Neurology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2211958
- DOI: http://doi.org/10.4174/jkss.2010.78.5.314
Abstract
- PURPOSE
The aim of this study was to compare the short and long-term outcomes following carotid endarterectomy (CEA) with either primary closure (PC) or patch angioplasty (PAT) performed by single center vascular surgeons.
METHODS
Between November 1994 and March 2008, a total of 366 patients underwent 401 consecutive primary CEA procedures at our institution. We retrospectively reviewed patients' medical records. Two vascular surgeons prefer routine PC and one vascular surgeon prefer routine patch closure using bovine pericardial patch. Postoperative neurologic complications were determined by clinical neurologists. Restenosis was defined as >50% stenosis on follow-up duplex scan. Data was analyzed to compare the early (< or =30 days) and late results of CEA between PC group and PAT group.
RESULTS
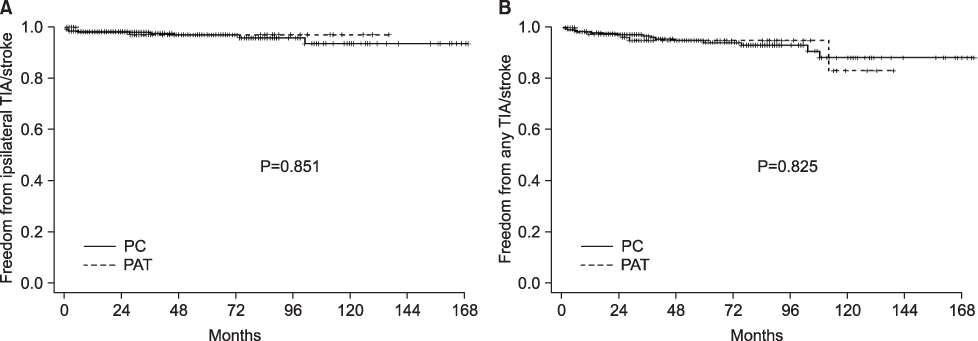
The mean follow-up duration was significantly longer in the PC group than that in the PAT group (61.7 months vs. 41.2 months, P<0.001). Coronary artery disease and combined CEA with coronary artery bypass were more common in the PAT group (39% vs. 55%, P<0.002; 4% vs. 12%, P<0.004). Perioperative ipsilateral TIA/stroke rates in the PC and PAT groups were 1.5% and 0.7% (PC=4/270 vs. PAT=1/131, P=0.564). Regarding late outcomes, Kaplan-Meier analysis failed to show any difference between 2 groups on freedom from ipsilateral transient ischemic attack (TIA)/stroke, freedom from restenosis and TIA/stroke-free survival (P=0.851, P=0.232, P=0.103, log-rank test).
CONCLUSION
Our results suggest that PC following CEA is not necessarily inferior to PAT for experienced surgeons.
MeSH Terms
Figure
Reference
-
1. Ranaboldo CJ, Barros D'Sa AA, Bell PR, Chant AD, Perry PM. The Joint Vascular Research Group. Randomized controlled trial of patch angioplasty for carotid endarterectomy. Br J Surg. 1993. 80:1528–1530.2. AbuRahma AF, Khan JH, Robinson PA, Saiedy S, Short YS, Boland JP, et al. Prospective randomized trial of carotid endarterectomy with primary closure and patch angioplasty with saphenous vein, jugular vein, and polytetrafluoroethylene: perioperative (30-day) results. J Vasc Surg. 1996. 24:998–1006.3. AbuRahma AF, Robinson PA, Saiedy S, Kahn JH, Boland JP. Prospective randomized trial of carotid endarterectomy with primary closure and patch angioplasty with saphenous vein, jugular vein, and polytetrafluoroethylene: long-term follow-up. J Vasc Surg. 1998. 27:222–232.4. Eikelboom BC, Ackerstaff RG, Hoeneveld H, Ludwig JW, Teeuwen C, Vermeulen FE, et al. Benefits of carotid patching: a randomized study. J Vasc Surg. 1988. 7:240–247.5. De Letter JA, Moll FL, Welten RJ, Eikelboom BC, Ackerstaff RG, Vermeulen FE, et al. Benefits of carotid patching: a prospective randomized study with long-term follow-up. Ann Vasc Surg. 1994. 8:54–58.6. Lord RS, Raj TB, Stary DL, Nash PA, Graham AR, Goh KH. Comparison of saphenous vein patch, polytetrafluoroethylene patch, and direct arteriotomy closure after carotid endarterectomy. Part I. Perioperative results. J Vasc Surg. 1989. 9:521–529.7. Katz D, Snyder SO, Gandhi RH, Wheeler JR, Gregory RT, Gayle RG, et al. Long-term follow-up for recurrent stenosis: a prospective randomized study of expanded polytetrafluoroethylene patch angioplasty versus primary closure after carotid endarterectomy. J Vasc Surg. 1994. 19:198–203.8. Clagett GP, Patterson CB, Fisher DF Jr, Fry RE, Eidt JF, Humble TH, et al. Vein patch versus primary closure for carotid endarterectomy. A randomized prospective study in a selected group of patients. J Vasc Surg. 1989. 9:213–223.9. Myers SI, Valentine RJ, Chervu A, Bowers BL, Clagett GP. Saphenous vein patch versus primary closure for carotid endarterectomy: long-term assessment of a randomized prospective study. J Vasc Surg. 1994. 19:15–22.10. Kim GE, Kwon TW, Cho YP, Kim HS. Carotid endarterectomy prospective study. J Korean Surg Soc. 1998. 55:265–273.11. Kim DI, Moon JY, Lee CH, Kim DY, Jang YS, Kim GM, et al. Primary closure after a carotid endarterectomy. Surg Today. 2007. 37:187–191.12. Liapis CD, Bell PR, Mikhailidis D, Sivenius J, Nicolaides A, Fernandes e Fernandes J, et al. ESVS guidelines. Invasive treatment for carotid stenosis: indications, techniques. Eur J Vasc Endovasc Surg. 2009. 37:1–19.13. Deriu GP, Ballotta E, Bonavina L, Grego F, Alvino S, Franceschi L, et al. The rationale for patch-graft angioplasty after carotid endarterectomy: early and long-term follow-up. Stroke. 1984. 15:972–979.14. Archie JP Jr. Prevention of early restenosis and thrombosisocclusion after carotid endarterectomy by saphenous vein patch angioplasty. Stroke. 1986. 17:901–905.15. AbuRahma AF, Robinson PA, Saiedy S, Richmond BK, Khan J. Prospective randomized trial of bilateral carotid endarterectomies: primary closure versus patching. Stroke. 1999. 30:1185–1189.16. Counsell C, Salinas R, Warlow C, Naylor R. Patch angioplasty versus primary closure for carotid endarterectomy. Cochrane Database Syst Rev. 2000. CD000160.17. Golledge J, Cuming R, Davies AH, Greenhalgh RM. Outcome of selective patching following carotid endarterectomy. Eur J Vasc Endovasc Surg. 1996. 11:458–463.18. Archie JP Jr. A fifteen-year experience with carotid endarterectomy after a formal operative protocol requiring highly frequent patch angioplasty. J Vasc Surg. 2000. 31:724–735.19. Byrne J, Feustel P, Darling RC 3rd. Primary closure, routine patching, and eversion endarterectomy: what is the current state of the literature supporting use of these techniques? Semin Vasc Surg. 2007. 20:226–235.20. Pearce WH, Parker MA, Feinglass J, Ujiki M, Manheim LM. The importance of surgeon volume and training in outcomes for vascular surgical procedures. J Vasc Surg. 1999. 29:768–776.21. Cowan JA Jr, Dimick JB, Thompson BG, Stanley JC, Upchurch GR Jr. Surgeon volume as an indicator of outcomes after carotid endarterectomy: an effect independent of specialty practice and hospital volume. J Am Coll Surg. 2002. 195:814–821.22. O'Hara PJ, Hertzer NR, Krajewski LP, Beven EG. Saphenous vein patch rupture after carotid endarterectomy. J Vasc Surg. 1992. 15:504–509.23. Borazjani BH, Wilson SE, Fujitani RM, Gordon I, Mueller M, Williams RA. Postoperative complications of carotid patching: pseudoaneurysm and infection. Ann Vasc Surg. 2003. 17:156–161.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Carotid Angioplasty: Is it Safe as Carotid Endarterectomy?
- Eversion Carotid Endarterectomy : A Short Review
- Carotid Endarterectomy Using Patch Angioplasty without Routine Completion Duplex Scan
- Current Indications of Surgery and Endovascular Treatment in Ischemic Stroke
- A Case of Transradial Approach to Carotid Artery Angioplasty and Stenting in Left Internal Carotid Stenosis