J Korean Soc Spine Surg.
2002 Dec;9(4):313-321. 10.4184/jkss.2002.9.4.313.
Outcome of Two Fusion Methods In Isthmic and Degenerative Spondylolisthesis of the Lumbar Spine
- Affiliations
-
- 1Department of Orthopaedic Surgery, College of Medicine, Dong-A University, Busan, Korea. gylee@mail.donga.ac.kr
- KMID: 2209713
- DOI: http://doi.org/10.4184/jkss.2002.9.4.313
Abstract
-
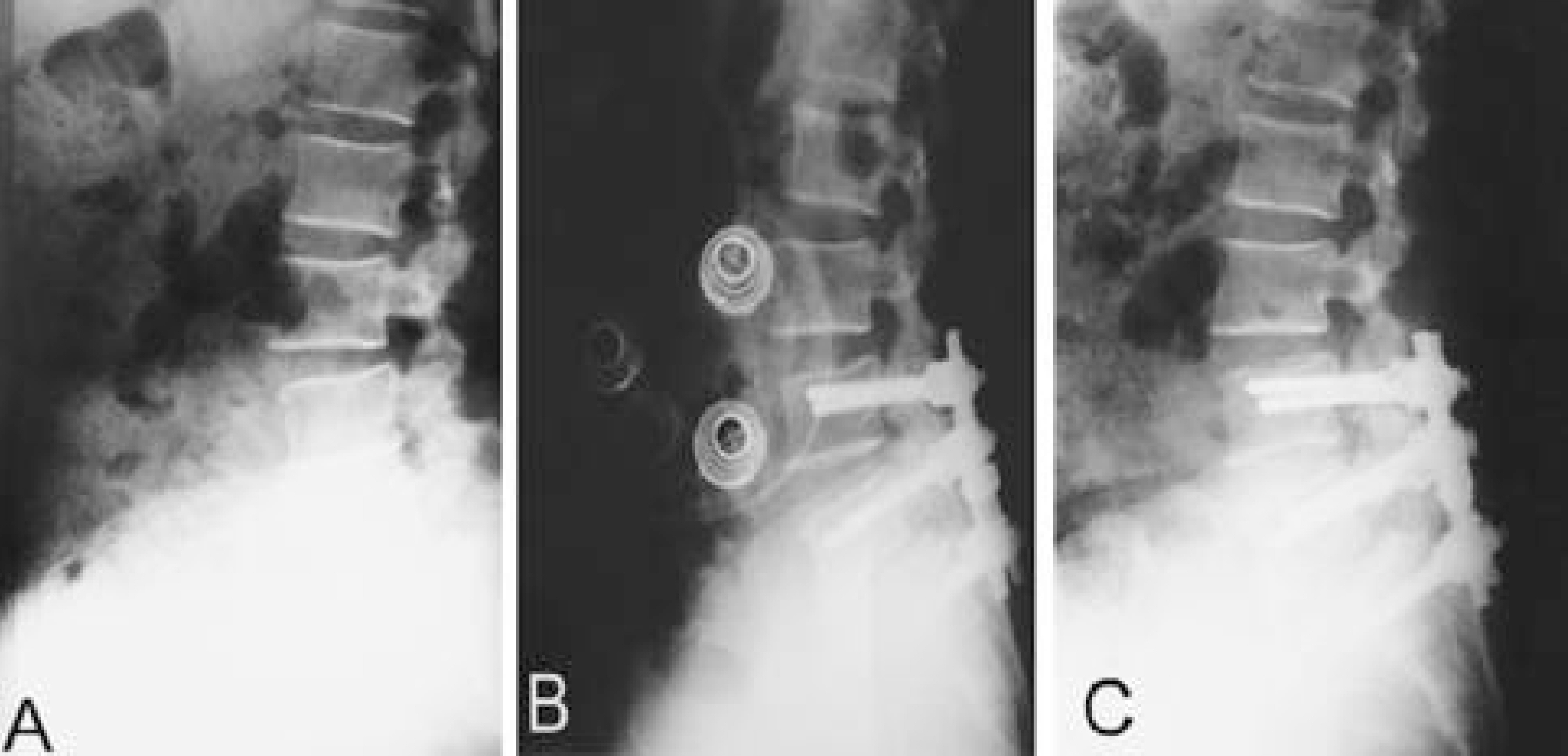
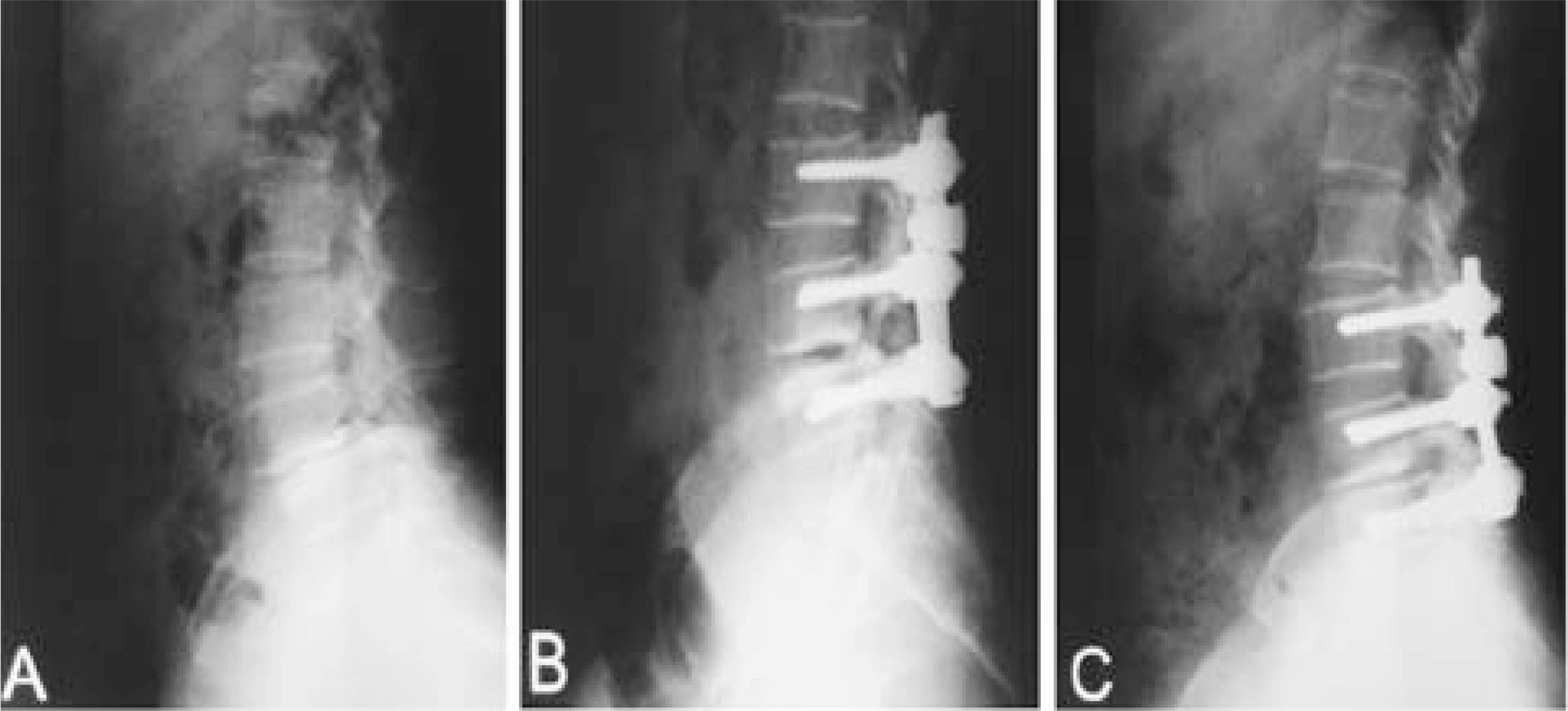
DESIGN: A retrospective study was performed in isthmic and degenerative spondylolisthesis patients who had undergone posterolateral fusion (PLF) only (group I) or posterolateral fusion (PLF) with posterior lumbar interbody fusion (PLIF) (group II).
OBJECTIVES
The objective of this study was to help in the selection of a surgical treatment option for spondylolisthesis. SUMMARY OF LITERATURE REVIEW: Irrespective of whether group Ior group II, satisfactory results have been reported in the surgical treatment of spondylolisthesis. However, isthmic and degenerative types have not been investigated in terms of outcome.
MATERIALS AND METHODS
We analyzed 112 patients (Isthmic: group I(32), group II(22), Degenerative: group I(37), group II(21)) who underwent surgical treatment for spondylolisthesis between April 1995 and December 2000. Kirkaldy-Willis criteria, radiologic union state, reduction ratio of slippage, change of disc space and change of segmental angle were analyzed as indicators of outcome.
RESULTS
We found the following by radiologic analysis: In isthmic spondylolisthesis, group IIwas better than group Iin terms of reduction ratio of slippage (reduction loss:3.38% vs. 2.3%, P=0.15), change of segmental angle (reduction loss : 2.11 degrees vs. 1.6degrees, P=0.15), bone union (83% vs. 92%, P=0.45) and change of disc space (reduction loss : 2.83 mm vs. 1.9 mm, P=0.02). In the degen-erative spondylolisthesis, group IIdid not show significant difference from group Iin terms of reduced slippage (reduction loss: 3.8% vs. 3.85%, P=0.47), change of segmental angle (reduction loss: 2.73 degrees vs. 2.64 degrees, P=0.43), bone union (80% vs. 87%, P=0.72) or disc height (reduction loss: 3.2 mm vs. 3.14 mm, P=0.45). In terms of clinical outcome, group II was better than groups Iin cases of isthmic spondylolisthesis (fair < or =:85% vs. 93%, P=0.72), however, groups IIwas not better than groups Iin cases of degenerative spondylolisthesis (fair < or =:83% vs. 85%, P=0.23).
CONCLUSIONS
In the degenerative spondylolisthesis patient, no significant difference was found between group Iand group II, but in the isthmic spondylolisthesis patient, group I and group II were found to be significantly different in terms of the reduction ratio of the disc heights.
Keyword
Figure
Reference
-
1). Boos N, Marchesi D, Zuber K and Aebi M. Treatment of severe spondylolisthesis by reduction and pedicular fixation: A 4-6 Year Follow Up Study. Spine. 18:1655–1661. 1993.2). Bridwell KG, Sedgewick TA, O’ Brien MF, Lenke LG and Baldus C. The role of fusion and instrumentation in the treatment of degenerative spondylolisthesis with spinal stenosis. J Spinal Disorder. 6:461–472. 1993.
Article3). Cho DY, Kim EH, Koh ES and Woo BC. The change of segmental sagittal angle in Low-grade spondylolisthesis after pedicular screw fixation with or without PLIF-PLIF+PLF versus PLF groups. J Korean Orthop Assoc. 30:842–851. 1995.4). Cloward RB. Posterior lumbar interbody fusion updated. Clin Orthop. 193:20–37. 1985.
Article5). Enker P and Steffee AD. Interbody fusion and instrumentation. Clin Orthop. 300:90–101. 1994.6). Esses S, Natout N and Kip P. Posterior interbody arthrodesis with a fibular strut graft in spondylolisthesis. J Bone Joint Surg. 77-A:172–176. 1995.
Article7). Esses SI, Sach BL and Dreyzin V. Complications associated with the technique of pedicle screw fixations. Spine. 18:2231–2239. 1993.8). Fredrickson BE, Baker D. Mcholick WJ, Yuan HA and Lubicky JP. The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg. 66-A:699–707. 1984.
Article9). Garfin SR. Summation. Spine. 19(20S):2300S–2305S. 1994.
Article10). Heim SE. Transpedicle instrumentation in the degenerative spine. Clin Orthop. 337:97–110. 1997.
Article11). Herkowitz HN and Kurz ST. Degenerative lumbar spondylolisthesis with spinal stenosis. J Bone Joint Surg. 72-A:802–808. 1991.12). Horowtch A, Peek RD, Thomas JC, Widell EH, Dimartino PP, Spencer CW, Weintein J and Wiltse LL. The pedicle screw fixation system, early clinical results. Spine. 14:461–467. 1989.13). Kim SS, Denis F, Lonstein JE and Winter RB. Factors affecting fusion rate in adult spondylolisthesis. Spine. 15:979–983. 1990.
Article14). Kirkaldy-Willis WH, Paine KWE and Cauchoiz J. Lumbar spinal stenosis. Clin Orthop. 99:30–52. 1974.15). Lenke LG, Birdwell KH, Bullis D, Betz RR, Baldus C and Schoenecker PL. Results of in situ fusion for isthmic spondylolisthesis. J Spinal Disorder. 5:433–441. 1992.
Article16). Lin PM. Posterior lumbar interbody fusion technique: Complication and pitfalls. Clin Orthop. 193:90–102. 1985.17). Lombardi JS, Wiltse LL, Reynolds J, Widell EH and Spencer C Ⅲ. Treatment of degenerative spondylolisthesis. Spine. 10:821–827. 1985.18). Lorenz M, Zindrick M, Schwaegler P, Vrbos L, Collatz MA, Behal R and Cram R. A comparison of single level fusions with and without hardware. Spine. 16:S455–S458. 1991.19). Ma GWC. Posterior lumbar interbody fusion with posterior elements as chip bone graft. Clin Orthop. 193:57–63. 1985.20). Matthiass HH and Heine J. The surgical reduction of spondylolisthesis. J Bone Joint Surg. 13:39–48. 1931.21). Newman PH and Stone KH. The etiology of spondylolisthesis. J Bone Joint Surg. 45-B:39–59. 1963.22). Steffee AD and Sitkowski DJ. Posterior lumbar interbody fustion and plates. Clin Orthop. 227:99–102. 1988.23). Suk SI, Lee CK, Kim WJ and Kim HG. Adding poste - rior lumbar interbody fusion to pedicle screw fixatin and posterolateral fusion after decompression in spondylolytic spondylolisthesis. J Korean Orthop Assoc. 30:1638–1646. 1995.24). Taillard W. Le Spondvloisthesis chez I'ecfant et I'adolescent. Acta Orthop Scand. 24:115. 1954.25). Valkenburg HA, Haanen HCM. The epidemiology of low back pain. In: White AA, Gordon SL, des, Proces Am Assoc Orthop Surg Symposium on Low Back Pain. 9–22. 1982.26). Verlooy J, De Smedt K and Selosse P. Failure of a modified posterior lumbar interbody fusion technique to produce adequate pain relief in isthmic spondylolytic grade l spondylolisthesis patients. Spine. 18:1491–1495. 1993.27). Wang JM, Kim DJ and Yun YH. Posterior pedicular screw instrumentation and anterior interbody fusion in adult lumbar spondylolysis or grade I spondyloilisthesis with segmental instability. J Spinal Disord. 9(2):83–8. 1996.28). Wiltse LL, Newman PH and Macnab I. Classification of spondylolysis and spondylolisthesis. Clin Orthop. 117:23–29. 1976.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Treatment of Degenerative and Isthmic Spondylolisthesis
- Comparison of Functional Outcomes following Surgical Decompression and Posterolateral Instrumented Fusion in Single Level Low Grade Lumbar Degenerative versus Isthmic Spondylolisthesis
- A Comparison of Surgical Treatment in Isthmic and Degenerative Spondylolisthesis
- Posterior Lumbar Interbody Fusion and Graf Band Fixation for Lumbar Isthmic Spondylolisthesis
- Posterior Fixation and Interbody for Lumbar Spondylolisthesis