J Korean Soc Radiol.
2010 Mar;62(3):227-234. 10.3348/jksr.2010.62.3.227.
MR Differentiation of Lung Cancer from Progressive Massive Fibrosis in Patients with Coal Worker's Pneumoconiosis
- Affiliations
-
- 1Department of Radiology, Seoul St. Mary's Hospital, The Catholic University of Korea, Korea. jijung@catholic.ac.kr
- 2Department of Occupational and Environmental Medicine, St. Mary's Hospital, The Catholic University of Korea, Korea.
- KMID: 2208917
- DOI: http://doi.org/10.3348/jksr.2010.62.3.227
Abstract
- PURPOSE
To analyze the potential of MR to distinguish lung cancer from progressive massive fibrosis (PMF) in patients with coal worker's pneumoconiosis.
MATERIALS AND METHODS
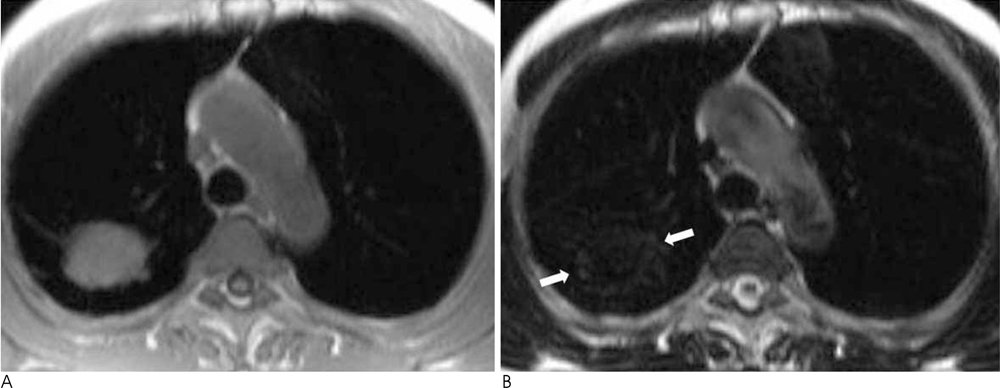
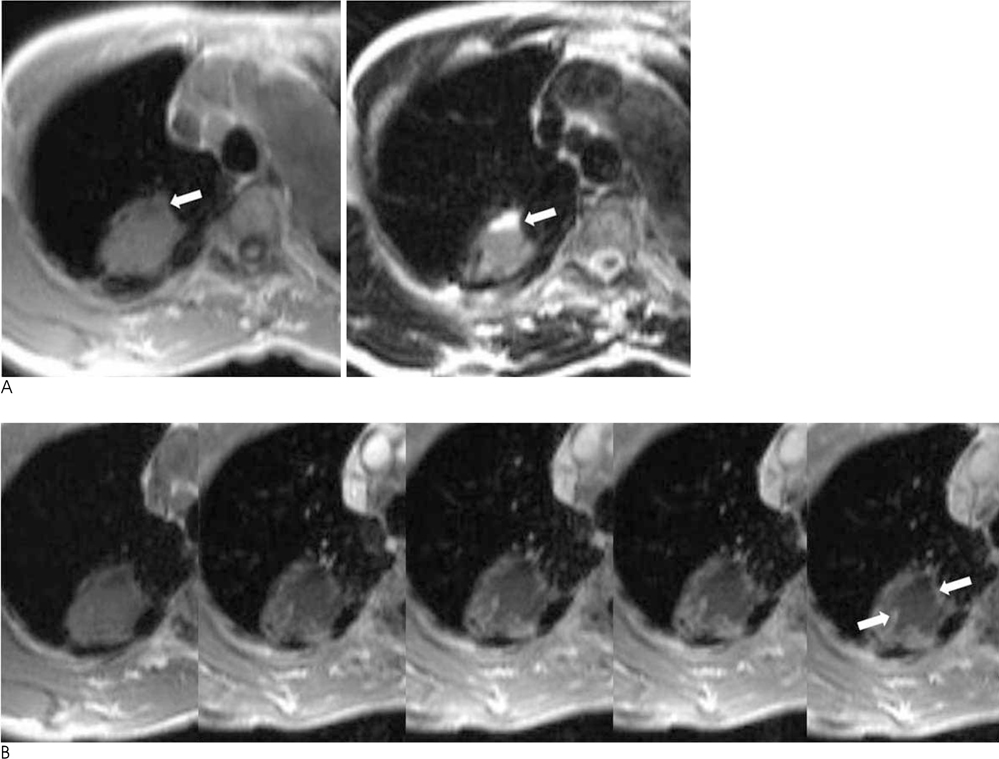
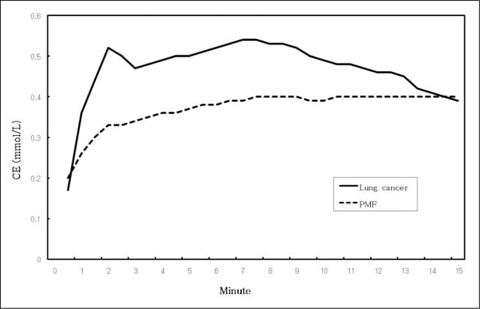
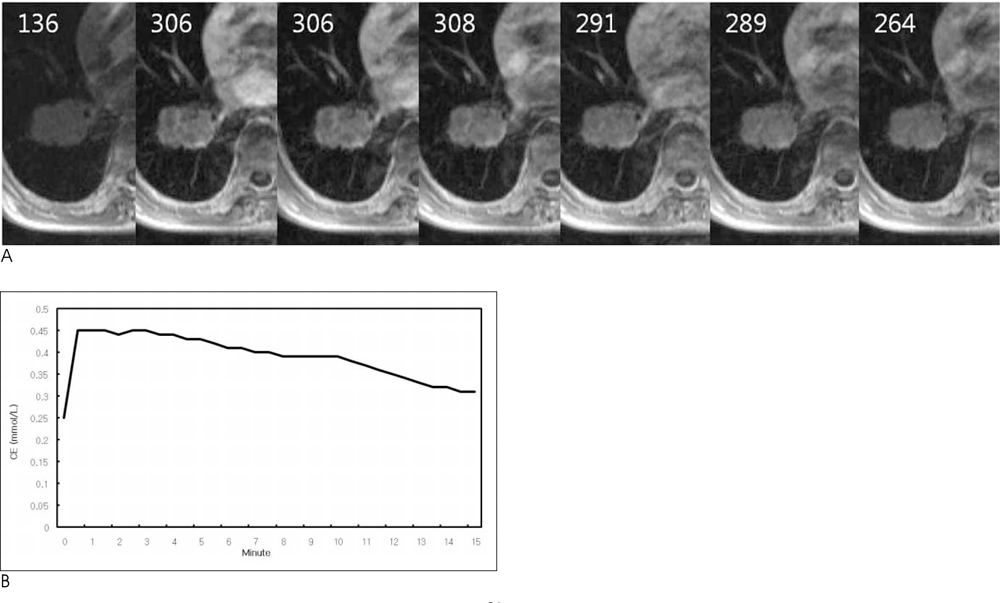
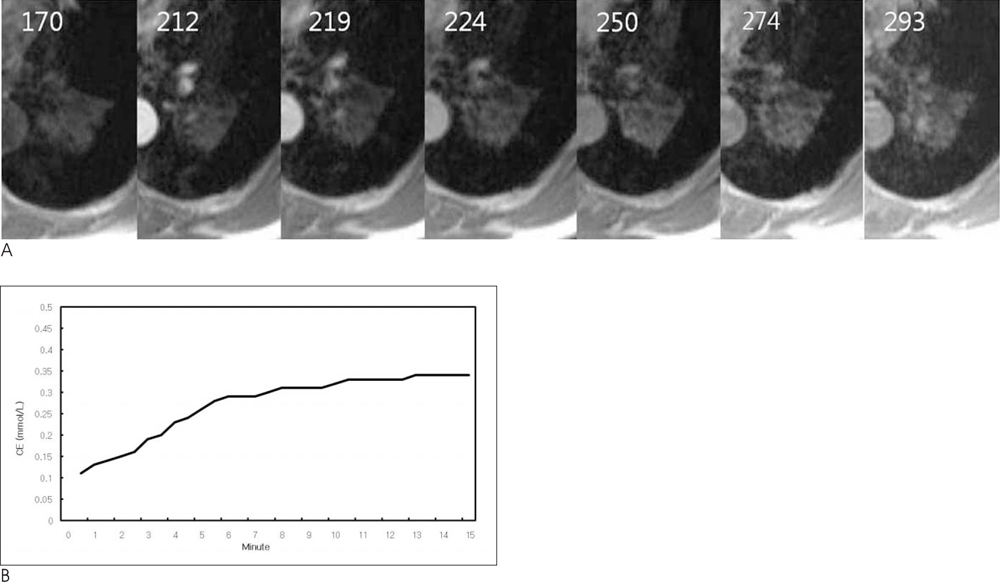
The study consisted of 9 patients with pathologically proven lung cancer and 26 PMFs in 17 patients. All the patients had radiologic evidence of pneumoconiosis. T1-weighted FLASH images were obtained before and 0.5, 1, 2, 3, 4, 5, 7.5, 10, 12.5, and 15 minutes after injection of Gd-DTPA. T2-weighted fast spin-echo images were obtained. The imaging findings were evaluated for enhancement time curve, contrast uptake equivalent (CE), and enhancement factor (EF).
RESULTS
On T1WI, there was no significant signal intensity difference between lung cancer and PMF. On T2WI, all lung cancer showed high signal intensity, as opposed to all PMFs which showed low signal intensity except for one PMF. Only one PMF showed high signal intensity on T2WI. For the dynamic contrast study, lung cancer showed faster and slightly stronger enhancement than PMFs. For a delayed image, most of the lung cancers (78%) showed washout, as opposed to a plateau in most of PMFs (73%) (p=0.0153). However, no difference was detected between the EFmax of lung cancer and PMFs (p=0.349).
CONCLUSION
MR is potentially a useful tool in distinguishing lung cancer from PMFs in patients with coal worker's pneumoconiosis.
MeSH Terms
Figure
Reference
-
1. Williams JL, Moler GA. Solitary mass in the lung of coal miners. Am J Roentgenol Radium Ther Nucl Med. 1973; 117:765–770.2. Stark P, Jacobson F, Shaffer K. Standard imaging in silicosis and coal worker’s pneumoconiosis. Radiol Clin North Am. 1992; 30:1147–1176.3. Matsumoto S, Miyake H, Oga M, Takaki H, Mori H. Diagnosis of lung cancer in a patient with pneumoconiosis and progressive massive fibrosis using MRI. Eur Radiol. 1998; 8:615–617.4. Hittmair K, Eckersberger F, Klepetko W, Helbich T, Herold CJ. Evaluation of solitary pulmonary nodules with dynamic contrastenhanced MR imaging-a promising technique? Magn Reson Imaging. 1995; 13:923–933.5. Rooke GB, Ward FG, Dempsey AN, Dowler JB, Whitaker CJ. Carcinoma of the lung in Lancashire coalminers. Thorax. 1979; 34:229–233.6. Ebihara I. A pathological study of carcinoma of the lung and pneumoconiosis. Nihon Kyobu Shikkan Gakkai Zasshi. 1989; 27:609–615.7. Kohout J, Motanova A, Sefrna F. Carcinoma of the lung in patient with pneumoconiosis. Vnitr Lek. 1993; 39:1044–1051.8. Lee SM, Kim TH, Lee JH, Ryu YH, Kim SJ. F-18 FDG PET Features of Progressive Massive Fibrosis in Patients with Pneumoconiosis. J Korean Radiol Soc. 2008; 59:255–260.9. Matsumoto S, Mori H, Miyake H, et al. MRI signal characteristics of progressive massive fibrosis in silicosis. Clin Radiol. 1998; 53:510–514.10. Jung JI, Park SH, Lee JM, Hahn ST, Kim KA. MR characteristics of progressive massive fibrosis. J Thorac Imaging. 2000; 15:144–150.11. Lee JK, Glazer HS. Controversy in the MR imaging appearance of fibrosis. Radiology. 1990; 177:21–22.12. Ebner F, Kressel HY, Mintz MC, Carlson JA, Cohen EK, Schiebler M. Tumor recurrence versus fibrosis in the female pelvis: differentiation with MR imaging at 1.5T. Radiology. 1988; 166:333–340.13. Shioya S, Haida M, Ono Y, Fukuazaki M, Yamabayashi H. Lung cancer: differentiation of tumor, necrosis, and atelectasis by means of T1 and T2 values measured in vitro. Radiology. 1988; 167:105–109.14. Kono R, Fujimoto K, Terasaki H, Muller NL, Kato S, Sadohara J. Dynamic MRI of solitary pulmonary nodules: Comparison of enhancement pattern of malignant and benign small peripheral lung lesions. AJR Am J Roentgenol. 2007; 188:26–36.15. Kwon W, Lee YH, Lee MS, Kim YJ, Sung KJ, Kim MS, Yong SJ, Jung SH. Usefulness of Perfusion CT in Progressive Massive Fibrosis. J Korean Radiol Soc. 2006; 54:69–77.16. Satoh S, Kitazume Y, Ohdama S, Kimula Y, Taura S, Endo Y. Can malignant and benign pulmonary nodules be differentiated with diffusion-weighted MRI? AJR Am J Roentgenol. 2008; 191:464–470.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Serum Lmmunoglobulin levels in Coal Worker's Pneumoconiosis Patients
- An Unusual Form of Progressive Massive Fibrosis In Pneumoconiosis
- Pulmonary Hemorrhage with Progressive Massive Fibrosis in a Silicosis Patient: An Autopsy Case
- Activity of Telomerase in Coal Worker's Autopsied Lung
- Clinical Significance of Plasma TGF-β1 in Coal Workers' Pneumoconiosis