J Korean Rheum Assoc.
2010 Dec;17(4):348-359. 10.4078/jkra.2010.17.4.348.
Clinical Approach of Common Foot and Ankle Disorders
- Affiliations
-
- 1Department of Orthopaedic Surgery, Konkuk University School of Medicine, Seoul, Korea. jungfoot@hanmail.net
- KMID: 2201892
- DOI: http://doi.org/10.4078/jkra.2010.17.4.348
Abstract
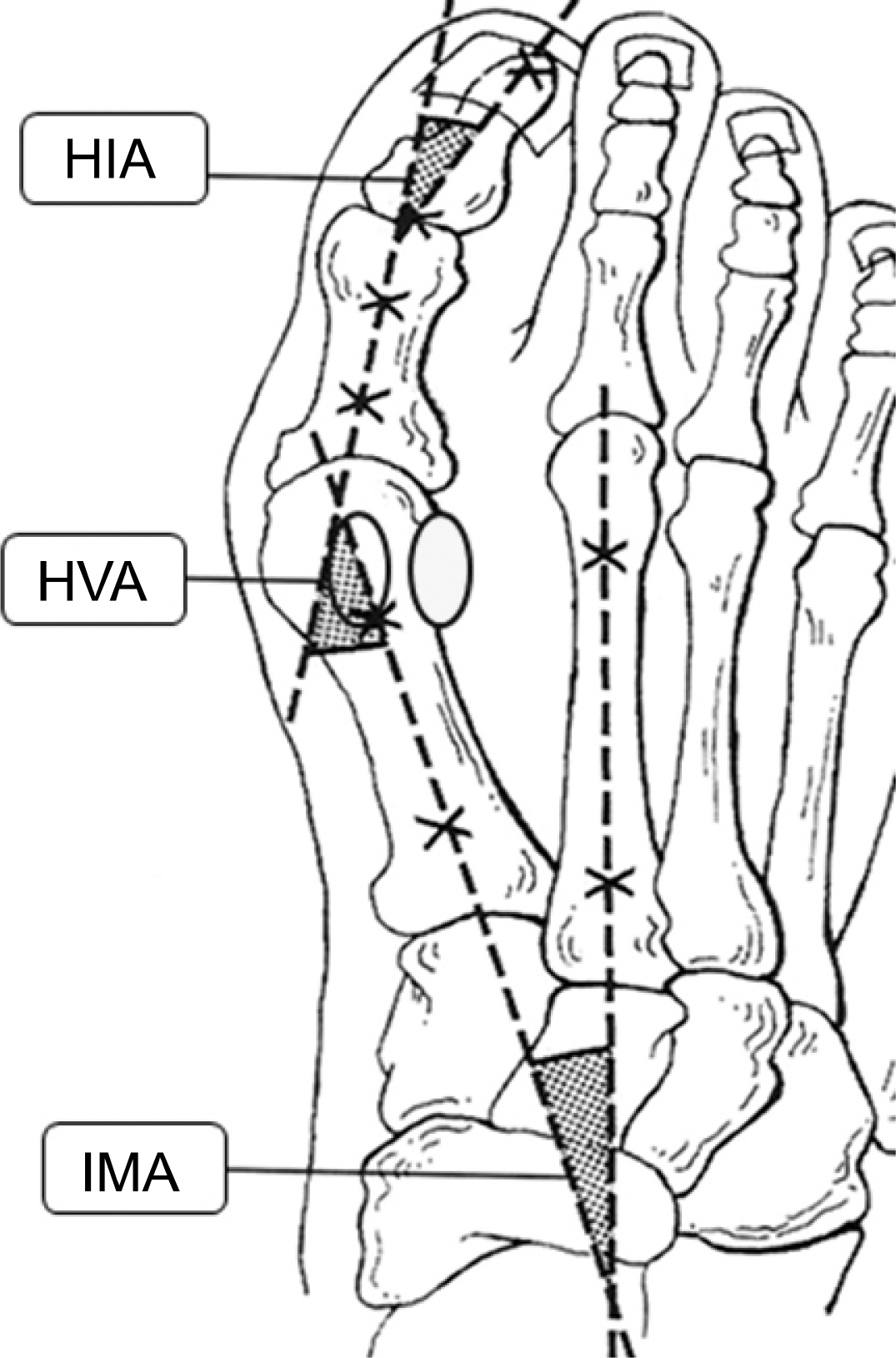
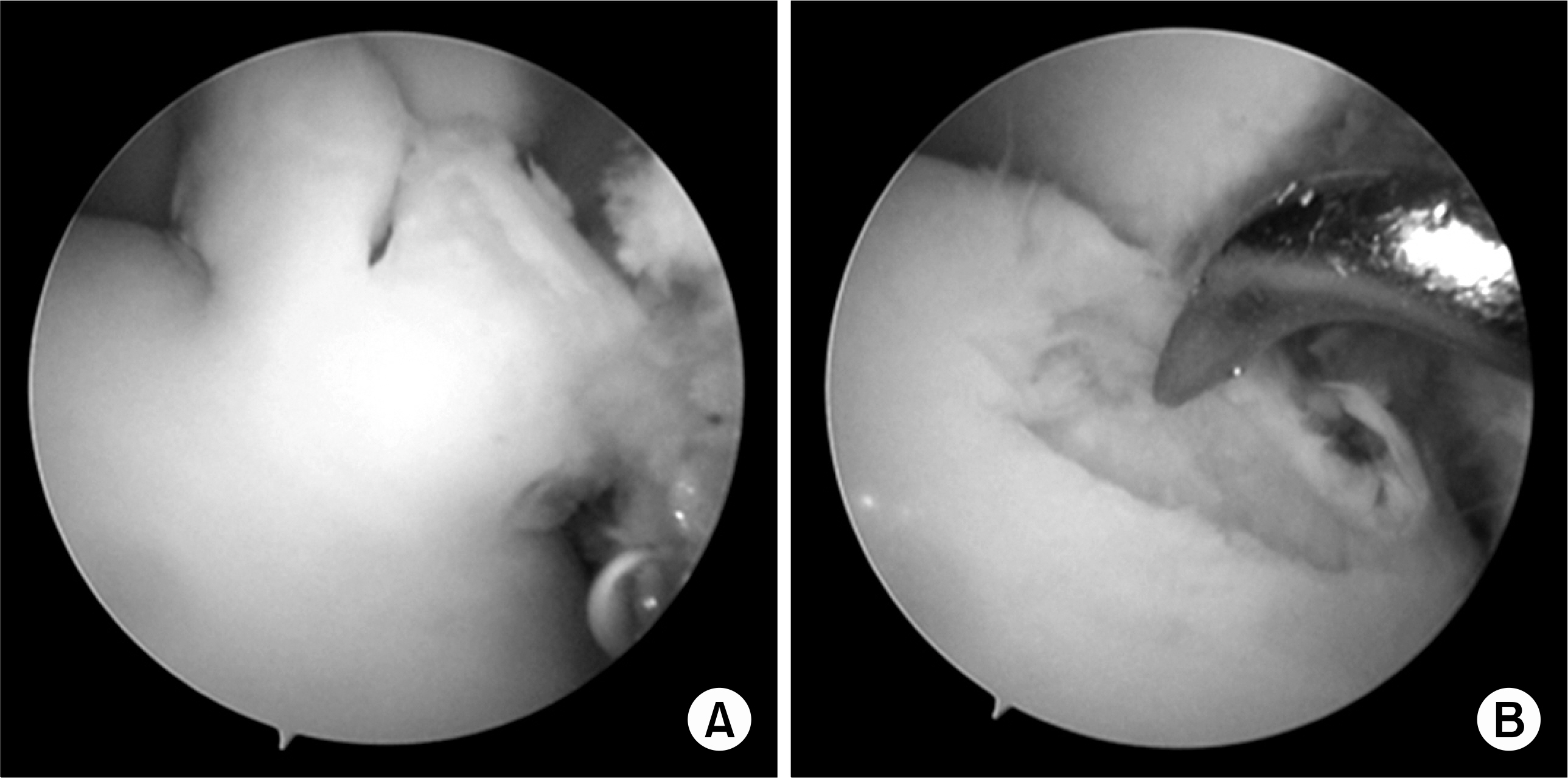
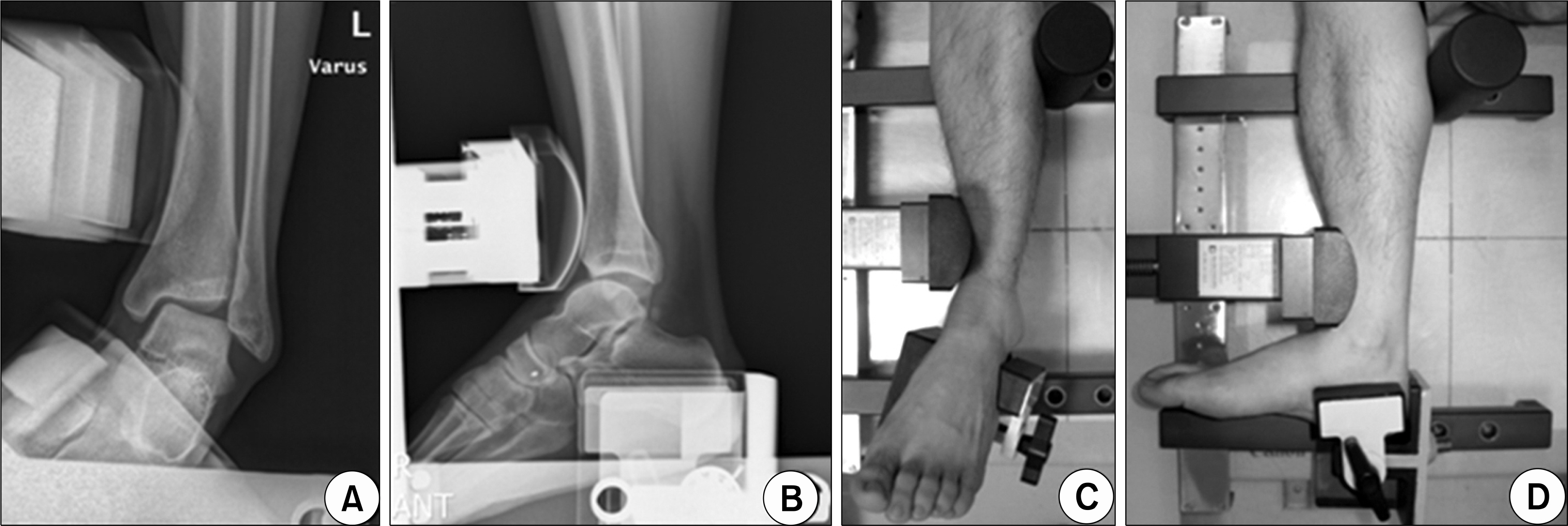
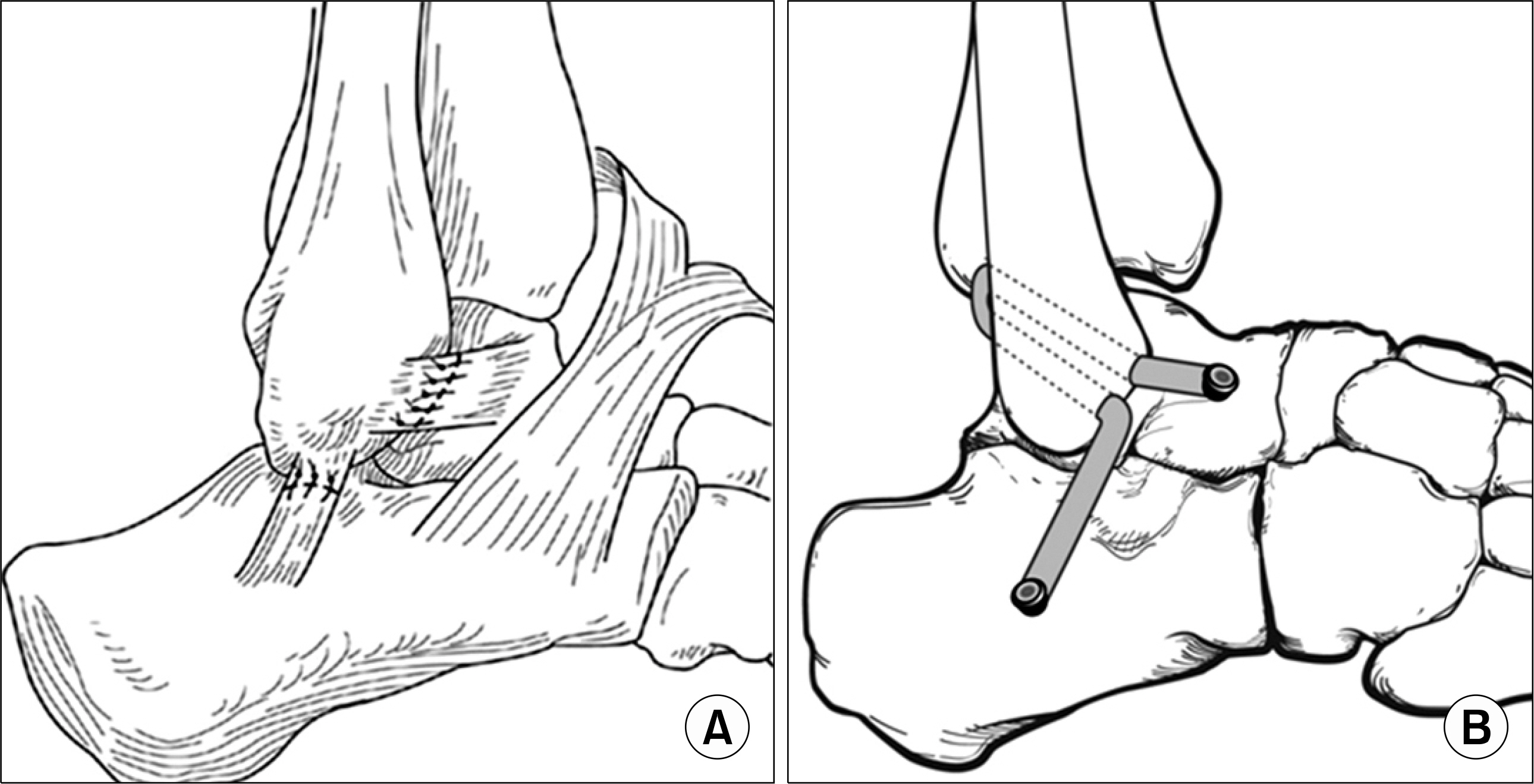
- Among the many regions (joints) of the human extremities, the foot and ankle area has a variety of disorders, which seem difficult to diagnose mainly because the anatomy seems rather complex. There are two main regions i.e. ankle and foot where the foot is divided into forefoot, midfoot and hindfoot. Among the many disorders, some of the most common and important disorders such as hallux valgus, osteochondral lesion of talus and lateral ankle instability are summarized in the aspect of clinical manifestations, physical examination, differential diagnosis, radiographic findings, initial treatments and the criteria for the surgery. The recent trend of surgical treatment options have also been described with related references.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Preoperative patient’s expectations and clinical outcomes after rheumatoid forefoot deformity reconstruction by joint sacrificing surgery
Sung-Jae Kim, Young-Woon Gil, Il-Hoon Sung
J Rheum Dis. 2024;31(1):33-40. doi: 10.4078/jrd.2023.0044.
Reference
-
1). Sammarco GJ., Russo-Alesi FG. Bunion correction using proximal chevron osteotomy: a singleincision technique. Foot Ankle Int. 1998. 19:430–7.
Article2). Easley ME., Trnka HJ. Current concepts review: hallux valgus part 1: pathomechanics, clinical assessment, and nonoperative management. Foot Ankle Int. 2007. 28:654–9.
Article3). Easley ME., Trnka HJ. Current concepts review: hallux valgus part II: operative treatment. Foot Ankle Int. 2007. 28:748–58.
Article4). Coughlin MJ., Shurnas PS. Hallux valgus in men. Part II: first ray mobility after bunionectomy and factors associated with hallux valgus deformity. Foot Ankle Int. 2003. 24:73–8.
Article5). Barouk LS. Scarf osteotomy for hallux valgus correction. Local anatomy, surgical technique, and combination with other forefoot procedures. Foot Ankle Clin. 2000. 5:525–58.6). Chiodo CP., Schon LC., Myerson MS. Clinical results with the Ludloff osteotomy for correction of adult hallux valgus. Foot Ankle Int. 2004. 25:532–6.
Article7). Verhagen RA., Maas M., Dijkgraaf MG., Tol JL., Krips R., van Dijk CN. Prospective study on diagnostic strategies in osteochondral lesions of the talus. Is MRI superior to helical CT? J Bone Joint Surg Br. 2005. 7:41–6.
Article8). O'Loughlin PF., Heyworth BE., Kennedy JG. Current concepts in the diagnosis and treatment of osteochondral lesions of the ankle. Am J Sports Med. 2010. 38:392–404.9). Berndt AL., Harty M. Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am. 1959. 41:988–1020.
Article10). Loomer R., Fisher C., Lloyd-Smith R., Sisler J., Cooney T. Osteochondral lesions of the talus. Am J Sports Med. 1993. 21:13–9.
Article11). Ferkel RD., Zanotti RM., Komenda GA., Sgaglione NA., Cheng MS., Applegate GR, et al. Arthroscopic treatment of chronic osteochondral lesions of the talus: long-term results. Am J Sports Med. 2008. 36:1750–62.12). Verhagen RA., Struijs PA., Bossuyt PM., van Dijk CN. Systematic review of treatment strategies for osteochondral defects of the talar dome. Foot Ankle Clin. 2003. 8:233–42.
Article13). Karlsson J., Lansinger O. Lateral instability of the ankle joint. Clin Orthop Relat Res. 1992. 276:253–61.
Article14). Peters JW., Trevino SG., Renstrom PA. Chronic lateral ankle instability. Foot Ankle. 1991. 12:182–91.
Article15). Komenda GA., Ferkel RD. Arthroscopic findings associated with the unstable ankle. Foot Ankle Int. 1999. 20:708–13.
Article16). McBride DJ., Ramamurthy C. Chronic ankle instability: management of chronic lateral ligamentous dysfunction and the varus tibiotalar joint. Foot Ankle Clin. 2006. 11:607–23.
Article17). DiGiovanni CW., Brodsky A. Current concepts: lateral ankle instability. Foot Ankle Int. 2006. 27:854–66.
Article18). Brostrom L. Sprained ankles. VI. Surgical treatment of “chronic” ligament ruptures. Acta Chir Scand. 1966. 132:551–65.19). Gould N., Seligson D., Gassman J. Early and late repair of lateral ligament of the ankle. Foot Ankle. 1980. 1:84–9.
Article20). Karlsson J., Bergsten T., Lansinger O., Peterson L. Surgical treatment of chronic lateral instability of the ankle joint. A new procedure. Am J Sports Med. 1989. 17:268–73.21). Burks RT., Morgan J. Anatomy of the lateral ankle ligaments. Am J Sports Med. 1994. 22:72–7.
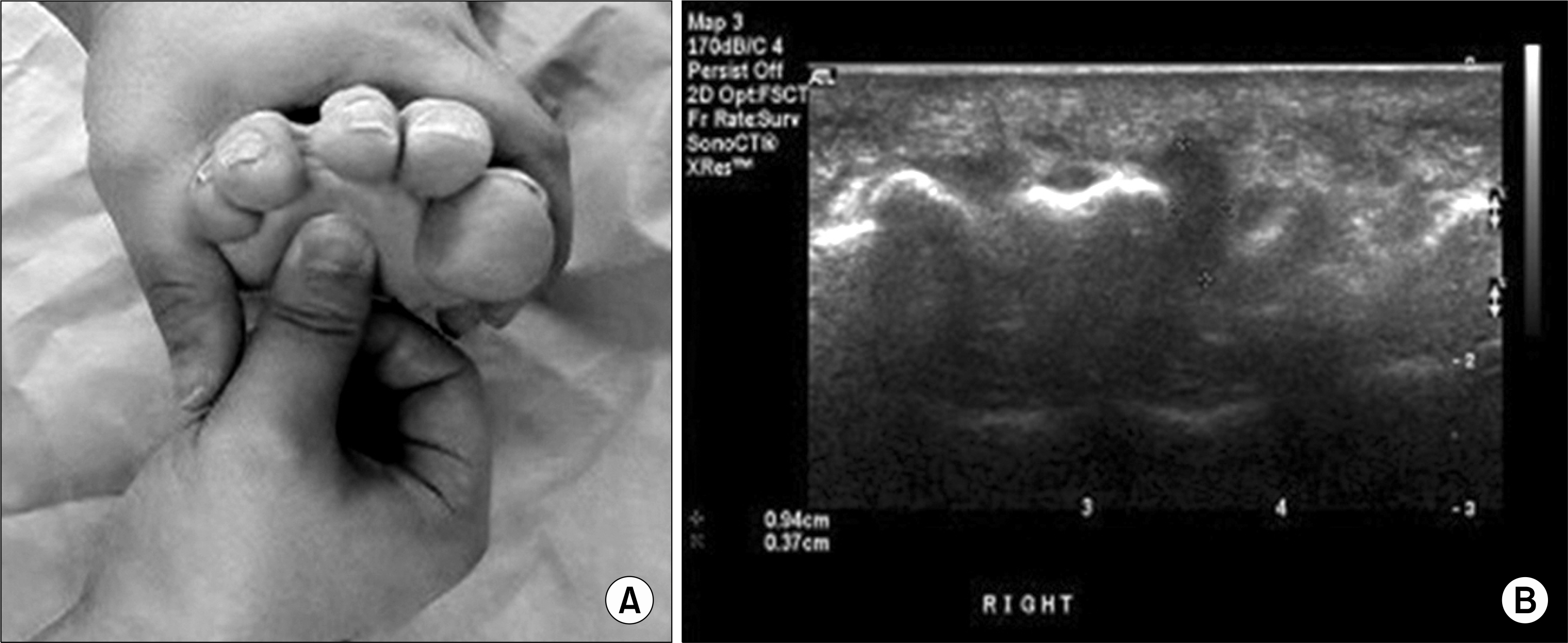
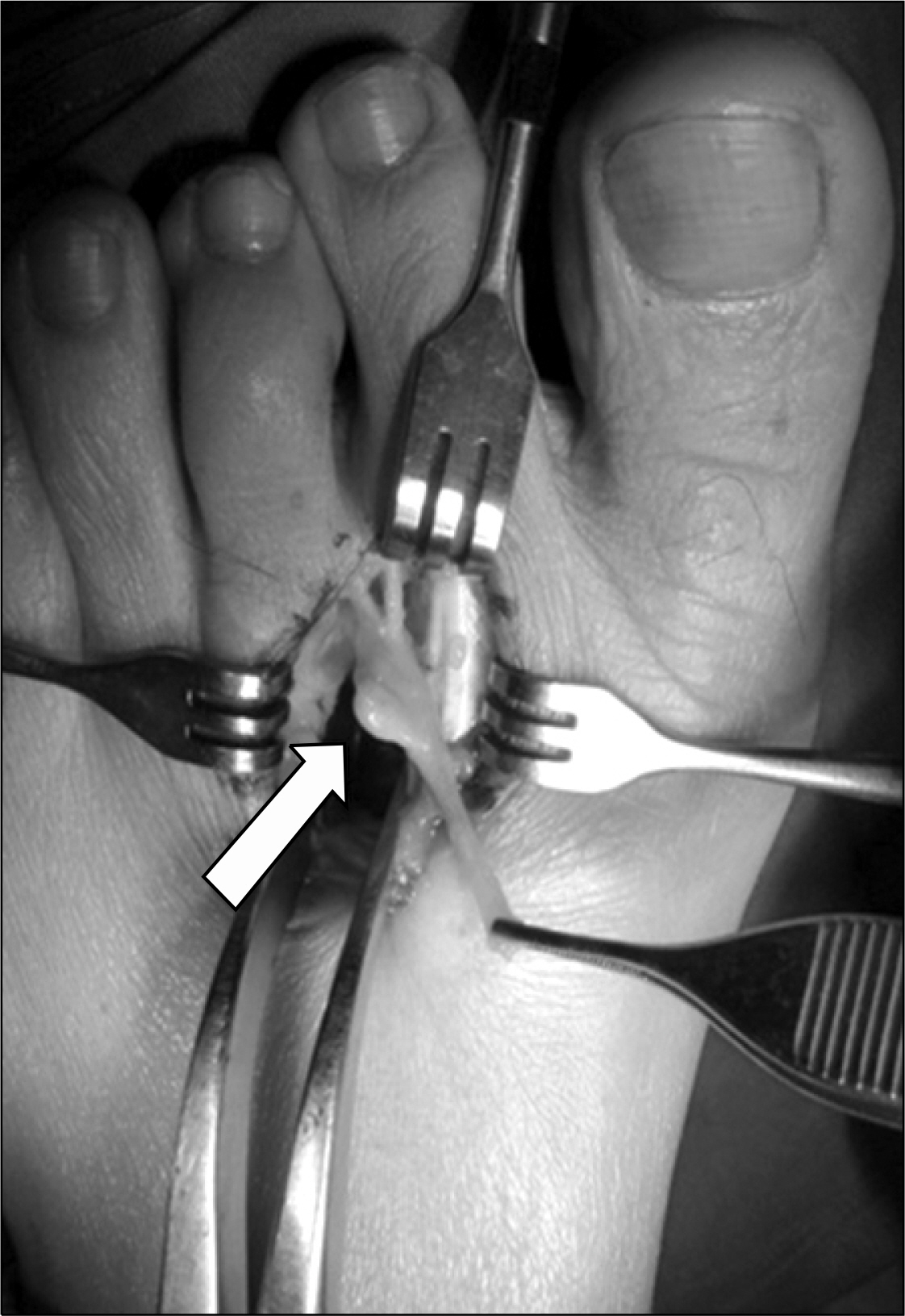
Article22). Guiloff RJ., Scadding JW., Klenerman L. Morton's metatarsalgia. Clinical, electrophysiological and histological observations. J Bone Joint Surg Br. 1984. 66:586–91.
Article23). Shapiro PP., Shapiro SL. Sonographic evaluation of interdigital neuromas. Foot Ankle Int. 1995. 16:604–6.
Article24). Saygi B., Yildirim Y., Saygi EK., Kara H., Esemenli T. Morton neuroma: comparative results of two conservative methods. Foot Ankle Int. 2005. 26:556–9.
Article25). Viladot A. Metatarsalgia due to biomechanical alterations of the forefoot. Orthop Clin North Am. 1973. 4:165–78.
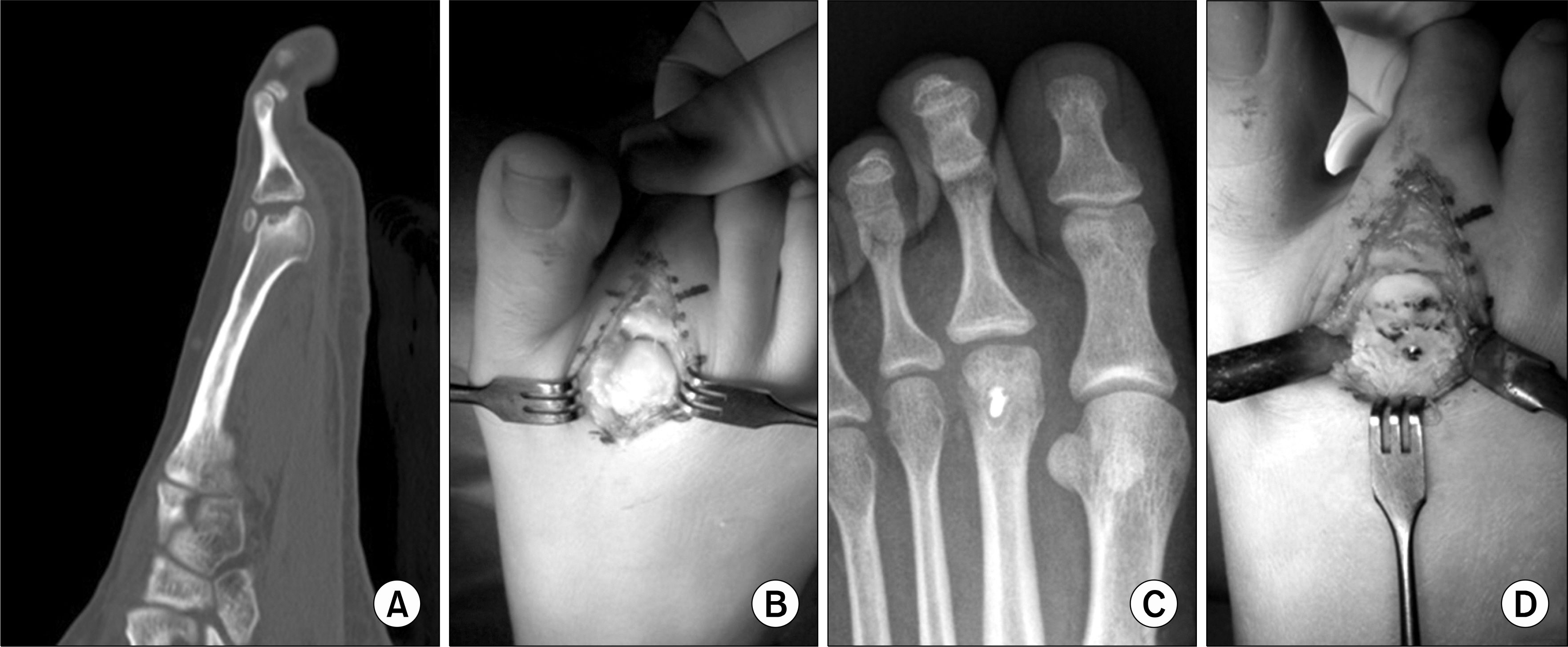
Article26). Carmont MR., Rees RJ., Blundell CM. Current concepts review: Freiberg's disease. Foot Ankle Int. 2009. 30:167–76.
Article27). Kinnard P., Lirette R. Freiberg's disease and dorsiflexion osteotomy. J Bone Joint Surg Br. 1991. 73:864–5.
Article