J Korean Radiol Soc.
1998 Mar;38(3):441-444. 10.3348/jkrs.1998.38.3.441.
Polyarteritis Nodosa in Superior Mesenteric Artery: A Case Report
- Affiliations
-
- 1Department of Radiology, Pathology, Hallym University College of Medicine.
- KMID: 2201399
- DOI: http://doi.org/10.3348/jkrs.1998.38.3.441
Abstract
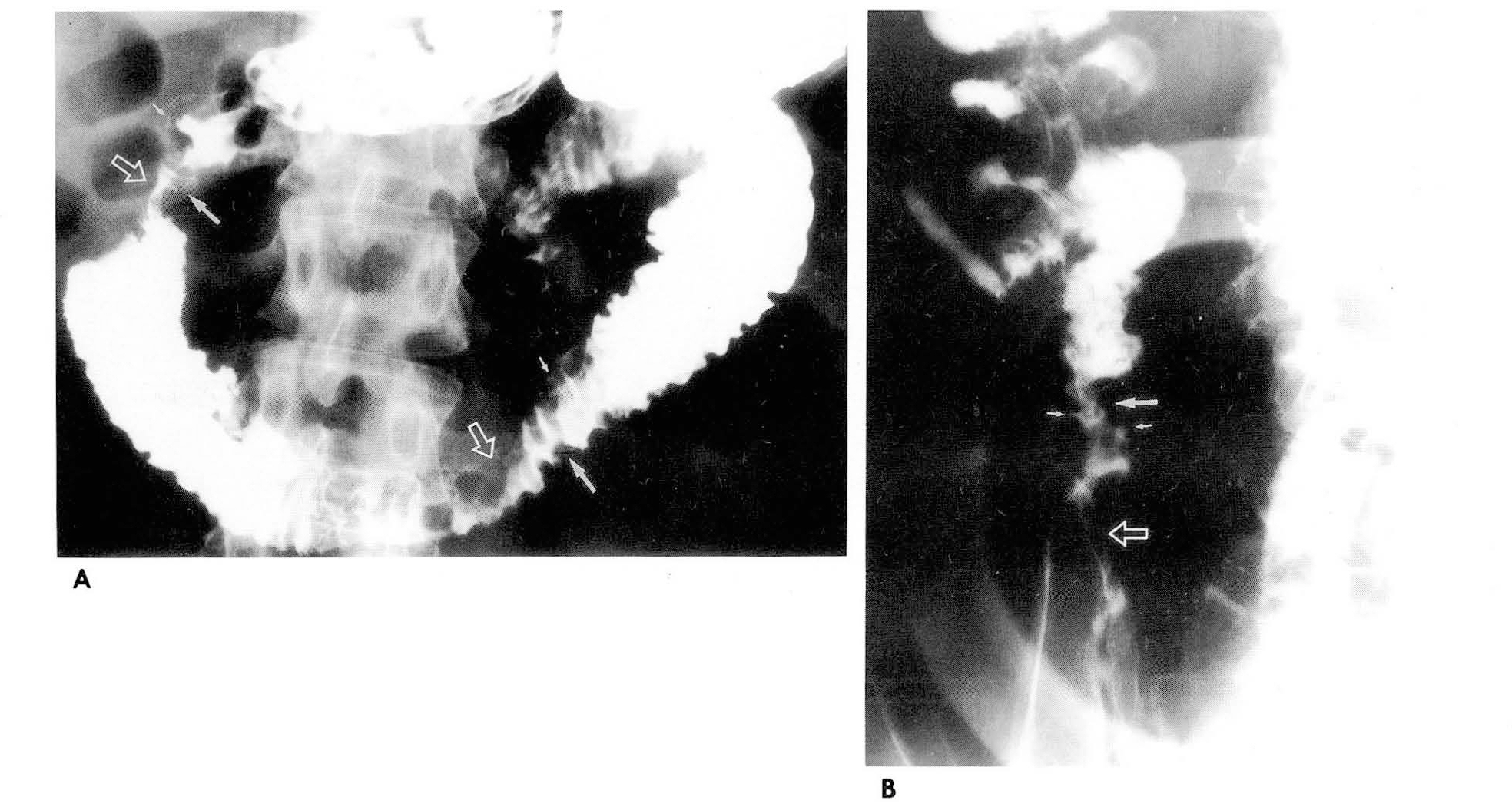
- Polyarteritis nodosa(PAN) is a multisystem disease characterized by necrotizing vasculitis of small andmedium-sized arteries, and in 50% of all cases there is gastrointestinal involvement. We describe a patient withPAN involving the gastrointestinal tract. A small bowel series showed nodular fold thickening, submucosal fillingdefects, shallow ulcerations, segmental luminal narrowing, and decreased peristalsis at the duodenum, jejunum, andileum; superior mesenteric arteriography showed hypervascularity and microaneurysm. Segmental resection of thesmall bowel indicated the presence of PAN.
Keyword
MeSH Terms
Figure
Reference
-
1.Kussmaul A., Maier Κ. Uber eine bischer nicht beschreibene eigenthumliche Arterienerkrankung (Polyarteritis nodosa), die mit Morbus Brightii und rapid fortschreitender allgemeiner Muskellahmung einhergeht. Dtsch Arch Klin Med. 1:484–517. 1866.2.Cupps T., Fauci A. The vasculitidis. In: Cupps TR, Fauci AS, eds. Major problems in internal medicine. Vol 21. Philadelphia: WB Saunders. 1981.3.Lopez L., Schocket A., Stanford R, et al. Gastrointestinal involvement in leukocytoclastic vasculitis and polyarteritis nodosa. J Rheumatol. 1980. 5:677–687.4.McCouley R., Johnston M., Fauci A. Surgical aspects of systemic necrotizing vasculitis. Surgery. 1985. 97:104–110.5.Spiegel R. Clinical aspects of periarteritis nodosa. Arch Intern Med. 1936. 58:993–1040.
Article6.C. Craig T, Barry M.B. Renal pathology with clinical correlation and functional correlations,. 2nd ed.Philadelphia: Lippincott;1993. p. 1990–1993.7.Halpern M., Citron BP. Necrotizing angiitis associated with drug abuse. AJR. 1971. 3:663–671.
Article8.Hekali P.., Kajander H.., Pajari R., et al. Diagnostic significance of angiographically observed visceral aneurysms with regard to polyarteritis nodosa. Acta Radiol. 1991. 32:143–148.
Article9.Marshak RH., Lindner AE. Radiology of the small intestine, ed 2. Philadelphia. 1976. WB Saunders.10.Craig RDP. Multiple perforations of the small intestine in polyarteritis nodosa. Gastroenterology. 1963. 44:355.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hybrid Surgery to Treat Multiple Visceral Aneurysms Secondary to Polyarteritis Nodosa
- Failure of Conservative Treatment in Two Cases of Polyarteritis Nodosa with Superior Mesenteric Artery Involvement Presenting with Abdominal Pain
- A case of polyarteritis nodosa with bilateral ureteral obstruction
- A Case of Polyarteritis Nodosa Associated with Central Retinal Artery Occlusion
- Polyangiitis overlap syndrome: cutaneous leukocytoclastic vasculitis associated with polyarteritis nodosa