J Korean Neurosurg Soc.
2015 Feb;57(2):100-107. 10.3340/jkns.2015.57.2.100.
Minimally Invasive Option Using Percutaneous Pedicle Screw for Instability of Metastasis Involving Thoracolumbar and Lumbar Spine : A Case Series in a Single Center
- Affiliations
-
- 1Department of Neurosurgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. sobotta72@hotmail.com
- 2Department of Orthopedic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2191190
- DOI: http://doi.org/10.3340/jkns.2015.57.2.100
Abstract
OBJECTIVE
To report a minimally invasive treatment option using percutaneous pedicle screw fixation with adjuvant treatment for metastatic thoraco-lumbar and lumbar spinal tumors.
METHODS
This is a retrospective study of charts of patients with spinal metastases. All were older than 18 years of age and were considered to have more than 3 months of life expectancy. The patients had single or two level lesions, and compression fracture or impending fracture. Exclusion criterion was metastasis showing severe epidural compression with definite neurological symptoms. Usually spinal segments from one level above to below pathology were stabilized. Visual analog scale (VAS) score for pain assessment and Frankel scale for neurological deficit were used, while pre- and post-operative performance status was evaluated using the Eastern Cooperative Oncology Group (ECOG).
RESULTS
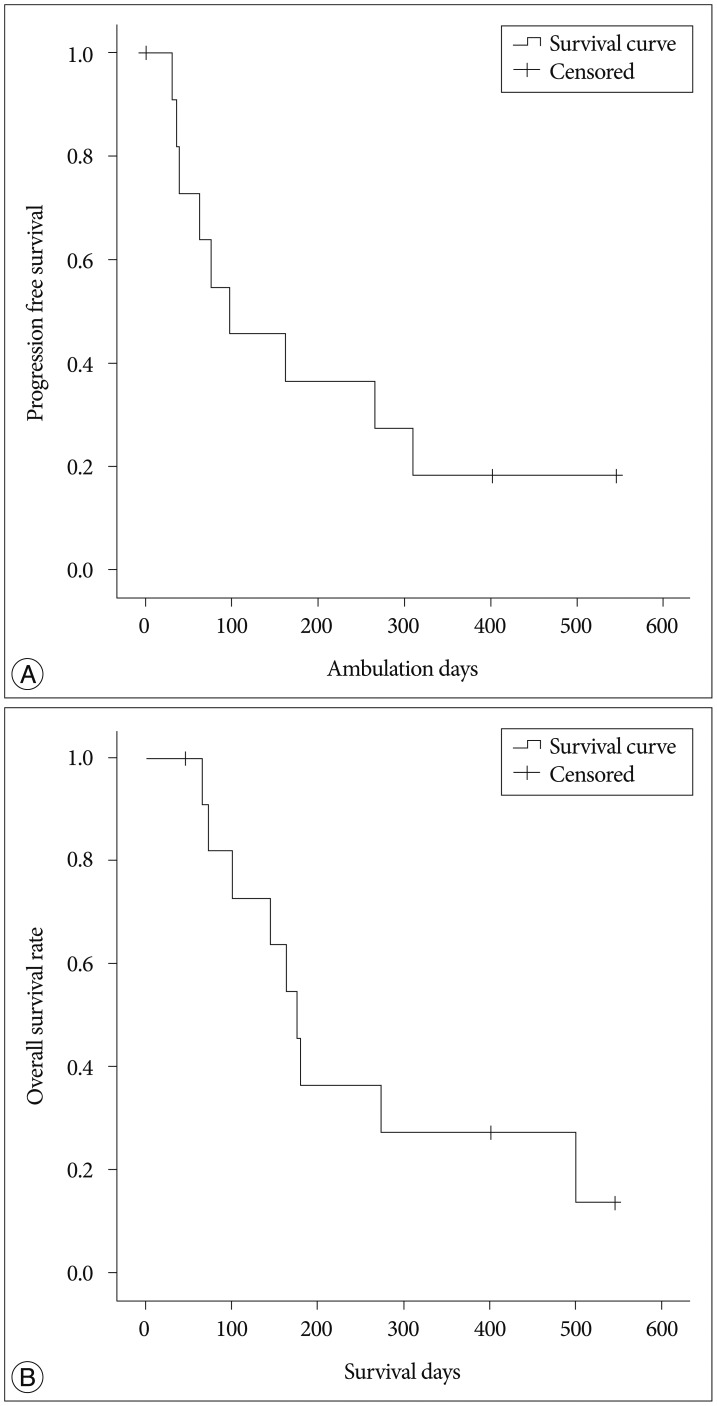
Twelve patients (nine men, three women; median age 54.29 years) underwent surgery. All patients presented with back pain with/without radicular pain. There were no early complications and perioperative mortalities. Following surgery, a significant difference between average pre- and post-operative VAS scores was found (p=0.003). Overall, 91.8% of patients (11/12) experienced improvement in their ECOG score post-operatively. The mean ambulation time was 196.9 days [95% confidence interval (CI), 86.2-307.6 days; median, 97 days]. During follow-up, nine patients died and the mean overall survival time in enrolled twelve patients was 249.9 days (95% CI, 145.3-354.4 days; median, 176 days).
CONCLUSION
Minimally invasive treatment using percutaneous pedicle screw fixation with adjuvant treatment is a good alternative treatment option for potential instability of the thoraco-lumbar and lumbar spinal metastasis.
MeSH Terms
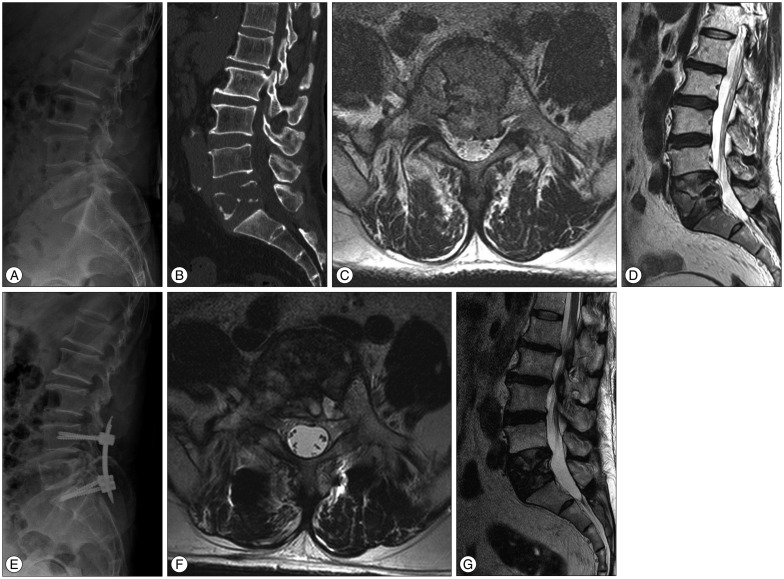
Figure
Cited by 1 articles
-
Bone Cement-Augmented Percutaneous Screw Fixation for Malignant Spinal Metastases: Is It Feasible?
Pius Kim, Seok Won Kim
J Korean Neurosurg Soc. 2017;60(2):189-194. doi: 10.3340/jkns.2016.0909.003.
Reference
-
1. Bailar JC 3rd, Gornik HL. Cancer undefeated. N Engl J Med. 1997; 336:1569–1574. PMID: 9164814.
Article2. Bartels RH, Feuth T, van der Maazen R, Verbeek AL, Kappelle AC, André Grotenhuis J, et al. Development of a model with which to predict the life expectancy of patients with spinal epidural metastasis. Cancer. 2007; 110:2042–2049. PMID: 17853394.
Article3. Cunha MV, Al-Omair A, Atenafu EG, Masucci GL, Letourneau D, Korol R, et al. Vertebral compression fracture (VCF) after spine stereotactic body radiation therapy (SBRT) : analysis of predictive factors. Int J Radiat Oncol Biol Phys. 2012; 84:e343–e349. PMID: 22658511.4. Di Martino A, Vincenzi B, Denaro L, Barnaba SA, Papalia R, Santini D, et al. 'Internal bracing' surgery in the management of solid tumor metastases of the thoracic and lumbar spine. Oncol Rep. 2009; 21:431–435. PMID: 19148519.
Article5. Falicov A, Fisher CG, Sparkes J, Boyd MC, Wing PC, Dvorak MF. Impact of surgical intervention on quality of life in patients with spinal metastases. Spine (Phila Pa 1976). 2006; 31:2849–2856. PMID: 17108840.
Article6. Fourney DR, Frangou EM, Ryken TC, Dipaola CP, Shaffrey CI, Berven SH, et al. Spinal instability neoplastic score : an analysis of reliability and validity from the spine oncology study group. J Clin Oncol. 2011; 29:3072–3077. PMID: 21709187.
Article7. Gerszten PC, Monaco EA 3rd. Complete percutaneous treatment of vertebral body tumors causing spinal canal compromise using a transpedicular cavitation, cement augmentation, and radiosurgical technique. Neurosurg Focus. 2009; 27:E9. PMID: 19951062.
Article8. Huang TJ, Hsu RW, Li YY, Cheng CC. Minimal access spinal surgery (MASS) in treating thoracic spine metastasis. Spine (Phila Pa 1976). 2006; 31:1860–1863. PMID: 16845365.
Article9. Ibrahim A, Crockard A, Antonietti P, Boriani S, Bünger C, Gasbarrini A, et al. Does spinal surgery improve the quality of life for those with extradural (spinal) osseous metastases? An international multicenter prospective observational study of 223 patients. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2007. J Neurosurg Spine. 2008; 8:271–278. PMID: 18312079.
Article10. Kim CH, Chung CK, Sohn S, Lee S, Park SB. Less invasive palliative surgery for spinal metastases. J Surg Oncol. 2013; 108:499–503. PMID: 23982866.
Article11. Le Huec JC, Lesprit E, Guibaud JP, Gangnet N, Aunoble S. Minimally invasive endoscopic approach to the cervicothoracic junction for vertebral metastases : report of two cases. Eur Spine J. 2001; 10:421–426. PMID: 11718197.
Article12. Mobbs RJ, Nakaji P, Szkandera BJ, Teo C. Endoscopic assisted posterior decompression for spinal neoplasms. J Clin Neurosci. 2002; 9:437–439. PMID: 12217675.
Article13. Patchell RA, Tibbs PA, Regine WF, Payne R, Saris S, Kryscio RJ, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer : a randomised trial. Lancet. 2005; 366:643–648. PMID: 16112300.
Article14. Rodríguez-Ruiz ME, San Miguel I, Gil-Bazo I, Perez-Gracia JL, Arbea L, Moreno-Jimenez M, et al. Pathological vertebral fracture after stereotactic body radiation therapy for lung metastases. Case report and literature review. Radiat Oncol. 2012; 7:50. PMID: 22455311.
Article15. Schneider F, Greineck F, Clausen S, Mai S, Obertacke U, Reis T, et al. Development of a novel method for intraoperative radiotherapy during kyphoplasty for spinal metastases (Kypho-IORT). Int J Radiat Oncol Biol Phys. 2011; 81:1114–1119. PMID: 20934272.
Article16. Singh K, Samartzis D, Vaccaro AR, Andersson GB, An HS, Heller JG. Current concepts in the management of metastatic spinal disease. The role of minimally-invasive approaches. J Bone Joint Surg Br. 2006; 88:434–442. PMID: 16567775.17. Tancioni F, Navarria P, Pessina F, Marcheselli S, Rognone E, Mancosu P, et al. Early surgical experience with minimally invasive percutaneous approach for patients with metastatic epidural spinal cord compression (MESCC) to poor prognoses. Ann Surg Oncol. 2012; 19:294–300. PMID: 21743979.
Article18. Thomas KC, Nosyk B, Fisher CG, Dvorak M, Patchell RA, Regine WF, et al. Cost-effectiveness of surgery plus radiotherapy versus radiotherapy alone for metastatic epidural spinal cord compression. Int J Radiat Oncol Biol Phys. 2006; 66:1212–1218. PMID: 17145536.
Article19. Tokuhashi Y, Matsuzaki H, Oda H, Oshima M, Ryu J. A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine (Phila Pa 1976). 2005; 30:2186–2191. PMID: 16205345.
Article20. Tomita K, Kawahara N, Murakami H, Demura S. Total en bloc spondylectomy for spinal tumors : improvement of the technique and its associated basic background. J Orthop Sci. 2006; 11:3–12. PMID: 16437342.
Article21. Weber BR, Grob D, Dvorák J, Müntener M. Posterior surgical approach to the lumbar spine and its effect on the multifidus muscle. Spine (Phila Pa 1976). 1997; 22:1765–1772. PMID: 9259789.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous Pedicle Screw Fixation in the Lumbar Spine
- Minimally Invasive Surgery for Fracture-dislocation of the Lumbar Spine with Neurologic Deficit and Hemodynamic Instability: A Case Report
- Minimally Invasive Spinal Stabilization Using Fluoroscopic-Guided Percutaneous Screws as a Form of Palliative Surgery in Patients with Spinal Metastasis
- Indirect decompression as a minimally invasive spine surgery
- Minimally Invasive Lumbar Decompression, Interbody Fusion, and Pedicle Screw Fixation: Preliminary Report