J Korean Neurosurg Soc.
2014 Jun;55(6):321-330. 10.3340/jkns.2014.55.6.321.
Surgical Experience of Infratentorial Meningiomas : Clinical Series at a Single Institution during the 20-Year Period
- Affiliations
-
- 1Department of Neurosurgery, Brain Tumor Clinic & Gamma Knife Center, Chonnam National University Research Institute of Medical Sciences, Chonnam National University Hwasun Hospital & Medical School, Hwasun, Korea. moonks@chonnam.ac.kr
- 2Department of Pathology, Brain Tumor Clinic & Gamma Knife Center, Chonnam National University Research Institute of Medical Sciences, Chonnam National University Hwasun Hospital & Medical School, Hwasun, Korea.
- KMID: 2191111
- DOI: http://doi.org/10.3340/jkns.2014.55.6.321
Abstract
OBJECTIVE
Based on surgical outcomes of patients with infratentorial meningiomas surgically treated at our institution, we analyzed the predictors for surgical resection, recurrence, complication, and survival.
METHODS
Of surgically treated 782 patients with intracranial meningioma, 158 (20.2%) consecutive cases of infratentorial location operated on between April 1993 and May 2013 at out institute were reviewed retrospectively. The patients had a median age of 57.1 years (range, 16--77 years), a female predominance of 79.7%, and a mean follow-up duration of 48.4 months (range, 0.8--242.2 months).
RESULTS
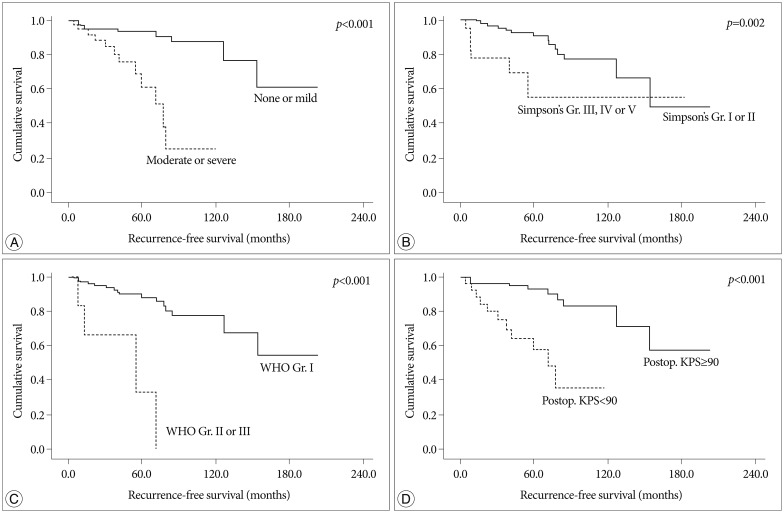
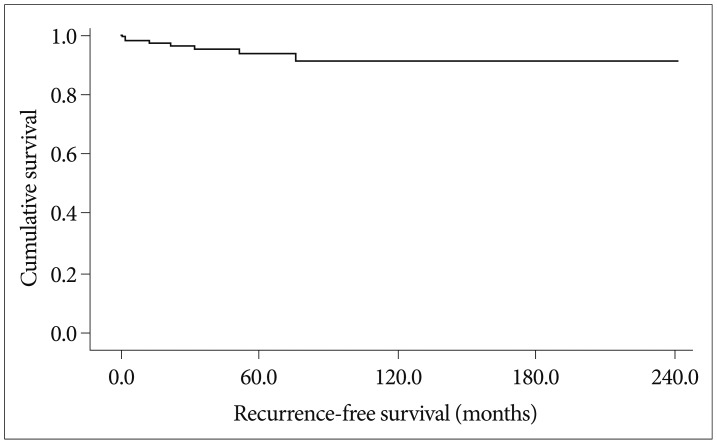
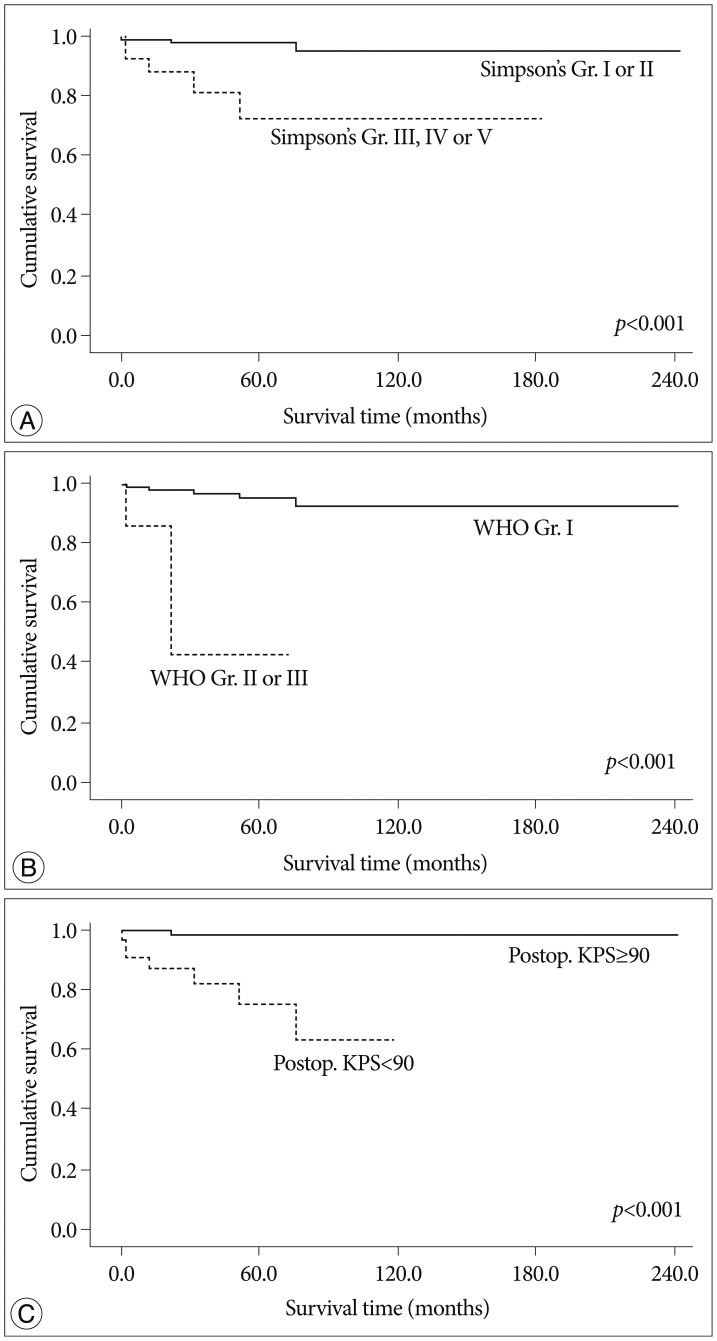
Gross total resection (Simpson's grade I & II) was achieved in 81.6% (129/158) of patients. Non-skull base location was an independent factor for complete resection. The recurrence rate was 13.3% (21/158) and the 5-, 10-, and 15-year recurrence rates were 8.2%, 12.0%, and 13.3%, respectively. Benign pathology, postoperative KPS over than 90, low peritumoral edema, and complete resection were significantly associated with longer recurrence-free survival rate. The 5-, 10-, and 15-year survival rates were 96.2%, 94.9%, and 94.9%, respectively. Benign pathology, postoperative KPS over than 90 and complete resection were significantly associated with a longer survival rate. The permanent complication rate was 13% (21/158). Skull base location and postoperative KPS less than 90 were independent factors for the occurrence of permanent complication.
CONCLUSION
Our experience shows that infratentorial meningiomas represent a continuing challenge for contemporary neurosurgeons. Various factors are related with resection degree, complications, recurrence and survival.
Keyword
MeSH Terms
Figure
Reference
-
1. Adegbite AB, Khan MI, Paine KW, Tan LK. The recurrence of intracranial meningiomas after surgical treatment. J Neurosurg. 1983; 58:51–56. PMID: 6847909.
Article2. Al-Mefty O, Fox JL, Smith RR. Petrosal approach for petroclival meningiomas. Neurosurgery. 1988; 22:510–517. PMID: 3362317.
Article3. Arienta C, Caroli M, Crotti F, Villani R. Treatment of intracranial meningiomas in patients over 70 years old. Acta Neurochir (Wien). 1990; 107:47–55. PMID: 2096608.
Article4. Ayerbe J, Lobato RD, de la Cruz J, Alday R, Rivas JJ, Gómez PA, et al. Risk factors predicting recurrence in patients operated on for intracranial meningioma. A multivariate analysis. Acta Neurochir (Wien). 1999; 141:921–932. PMID: 10526073.
Article5. Baroncini M, Thines L, Reyns N, Schapira S, Vincent C, Lejeune JP. Retrosigmoid approach for meningiomas of the cerebellopontine angle : results of surgery and place of additional treatments. Acta Neurochir (Wien). 2011; 153:1931–1940. discussion 1940. PMID: 21800106.
Article6. Bassiouni H, Hunold A, Asgari S, Stolke D. Meningiomas of the posterior petrous bone : functional outcome after microsurgery. J Neurosurg. 2004; 100:1014–1024. PMID: 15200116.
Article7. Bricolo AP, Turazzi S, Talacchi A, Cristofori L. Microsurgical removal of petroclival meningiomas : a report of 33 patients. Neurosurgery. 1992; 31:813–828. discussion 828. PMID: 1436406.8. Buhl R, Hasan A, Behnke A, Mehdorn HM. Results in the operative treatment of elderly patients with intracranial meningioma. Neurosurg Rev. 2000; 23:25–29. PMID: 10809483.
Article9. Castellano F, Ruggiero G. Meningiomas of the posterior fossa. Acta Radiol Suppl. 1953; 104:1–177. PMID: 13147998.10. Cornu P, Chatellier G, Dagreou F, Clemenceau S, Foncin JF, Rivierez M, et al. Intracranial meningiomas in elderly patients Postoperative morbidity and mortality Factors predictive of outcome. Acta Neurochir (Wien). 1990; 102:98–102. PMID: 2336986.11. Couldwell WT, Fukushima T, Giannotta SL, Weiss MH. Petroclival meningiomas : surgical experience in 109 cases. J Neurosurg. 1996; 84:20–28. PMID: 8613831.12. Cudlip SA, Wilkins PR, Johnston FG, Moore AJ, Marsh HT, Bell BA. Posterior fossa meningiomas : surgical experience in 52 cases. Acta Neurochir (Wien). 1998; 140:1007–1012. PMID: 9856243.13. Djindjian M, Caron JP, Athayde AA, Février MJ. Intracranial meningiomas in the elderly (over 70 years old) A retrospective study of 30 surgical cases. Acta Neurochir (Wien). 1988; 90:121–123. PMID: 3354358.14. Gerganov V, Bussarsky V, Romansky K, Popov R, Djendov S, Dimitrov I. Cerebellopontine angle meningiomas Clinical features and surgical treatment. J Neurosurg Sci. 2003; 47:129–135. discussion 135. PMID: 14618125.15. Gijtenbeek JM, Hop WC, Braakman R, Avezaat CJ. Surgery for intracranial meningiomas in elderly patients. Clin Neurol Neurosurg. 1993; 95:291–295. PMID: 8299286.
Article16. Jiang YG, Xiang J, Wen F, Zhang LY. Microsurgical excision of the large or giant cerebellopontine angle meningioma. Minim Invasive Neurosurg. 2006; 49:43–48. PMID: 16547882.
Article17. Kokkino AJ, Abdel Aziz KM, Tew JM Jr. Honored guest presentation : contemporary treatment of skull base meningiomas. Clin Neurosurg. 2000; 46:554–574. PMID: 10944701.18. Levine ZT, Buchanan RI, Sekhar LN, Rosen CL, Wright DC. Proposed grading system to predict the extent of resection and outcomes for cranial base meningiomas. Neurosurgery. 1999; 45:221–230. PMID: 10449065.
Article19. Lobato RD, Gonzaáez P, Alday R, Ramos A, Lagares A, Alen JF, et al. Meningiomas of the basal posterior fossa. Surgical experience in 80 cases. Neurocirugia (Astur). 2004; 15:525–542. PMID: 15632989.
Article20. Mayberg MR, Symon L. Meningiomas of the clivus and apical petrous bone. Report of 35 cases. J Neurosurg. 1986; 65:160–167. PMID: 3723172.21. Molony TB, Brackmann DE, Lo WW. Meningiomas of the jugular foramen. Otolaryngol Head Neck Surg. 1992; 106:128–136. PMID: 1738543.
Article22. Nakamura M, Roser F, Dormiani M, Vorkapic P, Samii M. Surgical treatment of cerebellopontine angle meningiomas in elderly patients. Acta Neurochir (Wien). 2005; 147:603–609. discussion 609-610. PMID: 15812593.
Article23. Papo I. Intracranial meningiomas in the elderly in the CT scan era. Acta Neurochir (Wien). 1983; 67:195–204. PMID: 6846076.
Article24. Proust F, Verdure L, Toussaint P, Bellow F, Callonec F, Menard JF, et al. [Intracranial meningioma in the elderly. Postoperative mortality, morbidity and quality of life in a series of 39 patients over 70 years of age]. Neurochirurgie. 1997; 43:15–20. PMID: 9205622.25. Roberti F, Sekhar LN, Kalavakonda C, Wright DC. Posterior fossa meningiomas : surgical experience in 161 cases. Surg Neurol. 2001; 56:8–20. discussion 20-21. PMID: 11546562.26. Samii M, Tatagiba M. Experience with 36 surgical cases of petroclival meningiomas. Acta Neurochir (Wien). 1992; 118:27–32. PMID: 1414527.
Article27. Sanna M, Bacciu A, Falcioni M, Taibah A, Piazza P. Surgical management of jugular foramen meningiomas : a series of 13 cases and review of the literature. Laryngoscope. 2007; 117:1710–1719. PMID: 17690614.
Article28. Sekhar LN, Swamy NK, Jaiswal V, Rubinstein E, Hirsch WE Jr, Wright DC. Surgical excision of meningiomas involving the clivus : preoperative and intraoperative features as predictors of postoperative functional deterioration. J Neurosurg. 1994; 81:860–868. PMID: 7965116.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiple Intracranial Meningiomas
- Long Term Clinical Outcomes of Malignant Meningiomas
- Surgical management of supratentorial and infratentorial epidural hematoma in Korea: three case reports
- Factors Influencing the Development of Peritumoral Brain Edema in Menigiomas
- Collision Tumors in Meningioma:Subtemporal Meningotheliomatous Meningioma and Subtemporal and Infratentorial Psammomatous Meningioma: Case Report