J Korean Neurosurg Soc.
2014 Feb;55(2):110-113. 10.3340/jkns.2014.55.2.110.
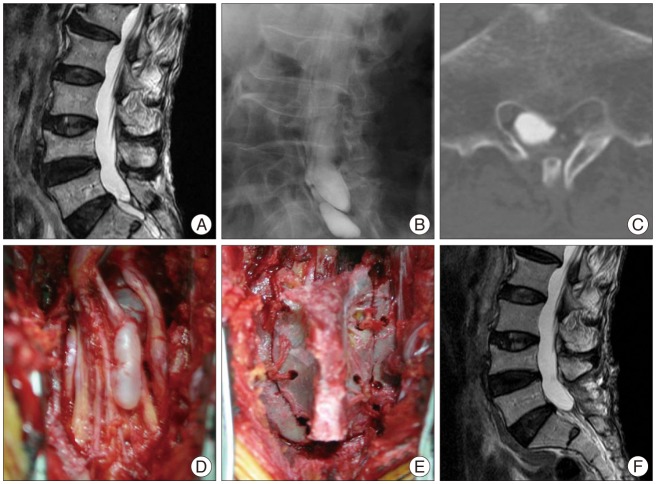
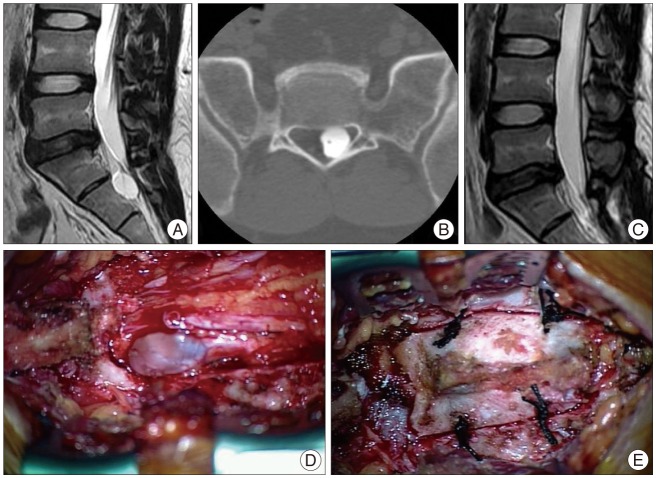
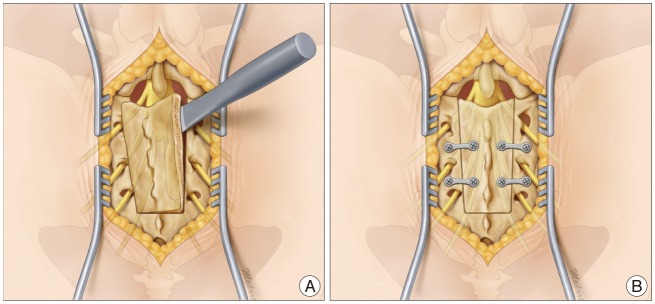
Microsurgical Excision of Symptomatic Sacral Perineurial Cyst with Sacral Recapping Laminectomy : A Case Report in Technical Aspects
- Affiliations
-
- 1Department of Neurosurgery, Dankook University College of Medicine, Cheonan, Korea. spine1225@naver.com
- KMID: 2191057
- DOI: http://doi.org/10.3340/jkns.2014.55.2.110
Abstract
- Perineurial cysts (Tarlov cysts) are lesions of the nerve root that are often observed in the sacral area. There is debate about whether symptomatic perineurial cysts should be treated surgically. We presented three patients with symptomatic perineurial cyst who were treated surgically, and introduced sacral recapping laminectomy. Patients complained of low back pain and hypesthesia on lower extremities. We performed operations with sacral recapping technique for all three. The outcome measure was baseline visual analogue score and post operative follow up magnetic resonance images. All patients were completely relieved of symptoms after operation. Although not sufficient to address controversies, this small case series introduces successful use of a particular surgical technique to treat sacral perineural cyst, with resolution of most symptoms and no sequelae.
Keyword
MeSH Terms
Figure
Reference
-
1. Bartels RH, van Overbeeke JJ. Lumbar cerebrospinal fluid drainage for symptomatic sacral nerve root cysts : an adjuvant diagnostic procedure and/or alternative treatment? Technical case report. Neurosurgery. 1997; 40:861–864. discussion 864-865. PMID: 9092864.2. Caspar W, Papavero L, Nabhan A, Loew C, Ahlhelm F. Microsurgical excision of symptomatic sacral perineurial cysts: a study of 15 cases. Surg Neurol. 2003; 59:101–105. discussion 105-106. PMID: 12648906.
Article3. Cattaneo L, Pavesi G, Mancia D. Sural nerve abnormalities in sacral perineural (Tarlov) cysts. J Neurol. 2001; 248:623–624. PMID: 11518008.
Article4. Dastur HM. The radiological appearances of spinal extradural arachnoid cysts. J Neurol Neurosurg Psychiatry. 1963; 26:231–235. PMID: 14025208.
Article5. Davis DH, Wilkinson JT, Teaford AK, Smigiel MR. Sciatica produced by a sacral perineurial cyst. Tex Med. 1987; 83:55–56. PMID: 3576493.6. Fortuna A, La Torre E, Ciappetta P. Arachnoid diverticula: a unitary approach to spinal cysts communicating with the subarachnoid space. Acta Neurochir (Wien). 1977; 39:259–268. PMID: 602855.
Article7. Hefti M, Landolt H. Presacral mass consisting of a meningocele and a Tarlov cyst: successful surgical treatment based on pathogenic hypothesis. Acta Neurochir (Wien). 2006; 148:479–483. PMID: 16322904.
Article8. Lim KT, Cho BM, Shin DI, Park SH, Oh SM. Symptomatic Tarlov's cyst (sacral meningeal cyst) case report. J Korean Neurosurg Soc. 2000; 29:569–573.9. Mummaneni PV, Pitts LH, McCormack BM, Corroo JM, Weinstein PR. Microsurgical treatment of symptomatic sacral Tarlov cysts. Neurosurgery. 2000; 47:74–78. discussion 78-79. PMID: 10917349.
Article10. Nabors MW, Pait TG, Byrd EB, Karim NO, Davis DO, Kobrine AI, et al. Updated assessment and current classification of spinal meningeal cysts. J Neurosurg. 1988; 68:366–377. PMID: 3343608.
Article11. Nishiura I, Koyama T, Handa J. Intrasacral perineurial cyst. Surg Neurol. 1985; 23:265–269. PMID: 3975809.
Article12. North RB, Kidd DH, Wang H. Occult, bilateral anterior sacral and intrasacral meningeal and perineurial cysts : case report and review of the literature. Neurosurgery. 1990; 27:981–986. PMID: 2274142.
Article13. Patel MR, Louie W, Rachlin J. Percutaneous fibrin glue therapy of meningeal cysts of the sacral spine. AJR Am J Roentgenol. 1997; 168:367–370. PMID: 9016209.
Article14. Paulsen RD, Call GA, Murtagh FR. Prevalence and percutaneous drainage of cysts of the sacral nerve root sheath (Tarlov cysts). AJNR Am J Neuroradiol. 1994; 15:293–297. discussion 298-299. PMID: 8192075.15. Tanaka M, Nakahara S, Ito Y, Nakanishi K, Sugimoto Y, Ikuma H, et al. Surgical results of sacral perineural (Tarlov) cysts. Acta Med Okayama. 2006; 60:65–70. PMID: 16508691.16. Tarlov IM. Perineurial cysts of the spinal nerve roots. Arch Neurol Psychiatry. 1938; 40:1067–1074.
Article