J Korean Neurosurg Soc.
2013 Dec;54(6):528-531. 10.3340/jkns.2013.54.6.528.
Successful Treatment of Infantile Fibrosarcoma Spinal Metastasis by Chemotherapy and Stereotactic Hypofractionated Radiotherapy
- Affiliations
-
- 1Department of Radiation Oncology, Tri-Service General Hospital, National Defense Medical Center, Taiwan, ROC. yeeminjen@gmail.com
- 2Department of Pediatrics, Tri-Service General Hospital, National Defense Medical Center, Taiwan, ROC.
- KMID: 2190953
- DOI: http://doi.org/10.3340/jkns.2013.54.6.528
Abstract
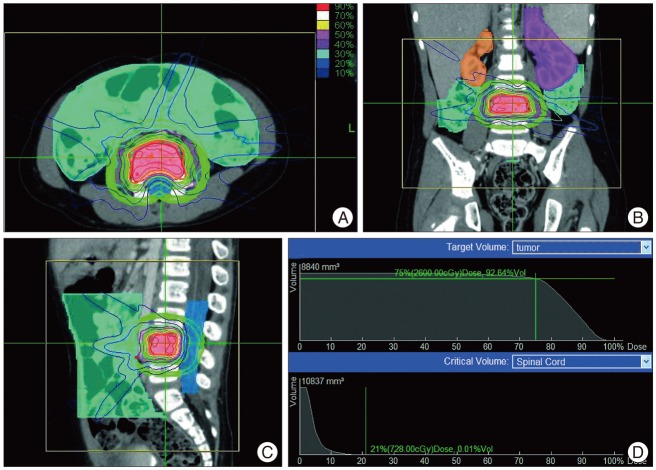
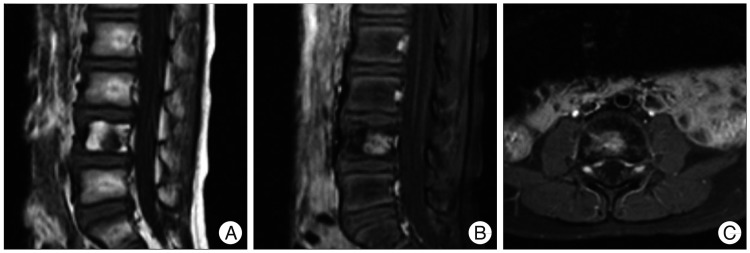
- We report a case of infantile fibrosarcoma in an 8-month-old boy manifested as a right-sided lower leg mass. Repeated local recurrence and distant metastasis were noted during the following three-year period. Whole body fluoro-deoxyglucose positron emission tomography scan revealed an asymptomatic metastasis involving the fourth lumbar vertebrae. The patient received chemotherapy (VAC regimen) with Cyberknife(R) stereotactic hypofractionated radiotherapy (26 Gy; 4 fractions). This treatment reduced tumor size by 23% without acute radiation toxicity even after 33 months. This case suggests that combining chemotherapy and this form of radiotherapy may be safe and effective against childhood spinal metastasis.
MeSH Terms
Figure
Reference
-
1. Chang UK, Youn SM, Park SQ, Rhee CH. Clinical results of cyberknife(r) radiosurgery for spinal metastases. J Korean Neurosurg Soc. 2009; 46:538–544. PMID: 20062569.
Article2. Diallo I, Haddy N, Adjadj E, Samand A, Quiniou E, Chavaudra J, et al. Frequency distribution of second solid cancer locations in relation to the irradiated volume among 115 patients treated for childhood cancer. Int J Radiat Oncol Biol Phys. 2009; 74:876–883. PMID: 19386434.
Article3. Fletcher CDM, Unni K, Mertens K. World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of Soft Tissue and Bone. Lyon: IARC Press;2002.4. Garg AK, Wang XS, Shiu AS, Allen P, Yang J, McAleer MF, et al. Prospective evaluation of spinal reirradiation by using stereotactic body radiation therapy : The University of Texas MD Anderson Cancer Center experience. Cancer. 2011; 117:3509–3516. PMID: 21319143.
Article5. Gerszten PC, Burton SA, Ozhasoglu C, Welch WC. Radiosurgery for spinal metastases : clinical experience in 500 cases from a single institution. Spine (Phila Pa 1976). 32:2007; 193–199. PMID: 17224814.6. Gibbs IC, Patil C, Gerszten PC, Adler JR Jr, Burton SA. Delayed radiation-induced myelopathy after spinal radiosurgery. Neurosurgery. 2009; 64(2 Suppl):A67–A72. PMID: 19165076.
Article7. Giller CA, Berger BD, Gilio JP, Delp JL, Gall KP, Weprin B, et al. Feasibility of radiosurgery for malignant brain tumors in infants by use of image-guided robotic radiosurgery : preliminary report. Neurosurgery. 2004; 55:916–924. discussion 924-925. PMID: 15458600.8. Giller CA, Berger BD, Pistenmaa DA, Sklar F, Weprin B, Shapiro K, et al. Robotically guided radiosurgery for children. Pediatr Blood Cancer. 2005; 45:304–310. PMID: 15558704.
Article9. Hall EJ, Brenner DJ. The radiobiology of radiosurgery : rationale for different treatment regimes for AVMs and malignancies. Int J Radiat Oncol Biol Phys. 1993; 25:381–385. PMID: 8420891.
Article10. Hall WA, Stapleford LJ, Hadjipanayis CG, Curran WJ, Crocker I, Shu HK. Stereotactic body radiosurgery for spinal metastatic disease : an evidence-based review. Int J Surg Oncol. 2011; 2011:979214. PMID: 22312536.11. Kerl K, Nowacki M, Leuschner I, Masjosthusmann K, Frühwald MC. Infantile fibrosarcoma - an important differential diagnosis of congenital vascular tumors. Pediatr Hematol Oncol. 2012; 29:545–548. PMID: 22812410.
Article12. Orbach D, Rey A, Cecchetto G, Oberlin O, Casanova M, Thebaud E, et al. Infantile fibrosarcoma : management based on the European experience. J Clin Oncol. 2010; 28:318–323. PMID: 19917847.13. Peugniez C, Dewas S, Coche-Dequéant B, Leblond P, Defachelles AS, Thebaud E, et al. Use of conventional fractionation with cyberknife in children : a report of 5 cases. J Pediatr Hematol Oncol. 2010; 32:472–475. PMID: 20588196.
Article14. Ramuz O, Bourhis J, Mornex F. [Late effects of radiations on mature and growing bone]. Cancer Radiother. 1997; 1:801–809. PMID: 9614899.15. Shah NN, Price MR, Loeb DM. Cardiac metastasis and hypertrophic osteoarthropathy in recurrent infantile fibrosarcoma. Pediatr Blood Cancer. 2012; 59:179–181. PMID: 21853519.
Article16. Sinha AK, Seki JT, Moreau G, Ventureyra E, Letts RM. The management of spinal metastasis in children. Can J Surg. 1997; 40:218–226. PMID: 9194784.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Updated Review on the Treatment Strategy for Spinal Metastasis from the Spine Surgeon’s Perspective
- Infantile Fibrosarcoma: A case report
- The mixed era of stereotactic radiosurgery and radiotherapy
- STRATOS Titanium Rib Bridge for Chest Wall Reconstruction after Infantile Fibrosarcoma Resection: A Case Report
- Infantile Fibrosarcoma in Neonate