J Korean Neurosurg Soc.
2012 Jul;52(1):62-66. 10.3340/jkns.2012.52.1.62.
Clinical and Radiological Findings of Nerve Root Herniation after Discectomy of Lumbar Disc Herniation
- Affiliations
-
- 1Department of Neurosurgery, Wooridul Spine Hospital, Seoul, Korea. spinejjs@yahoo.co.kr
- 2Department of Neurosurgery, Seoul Wooridul Hospital, Seoul, Korea.
- KMID: 2190527
- DOI: http://doi.org/10.3340/jkns.2012.52.1.62
Abstract
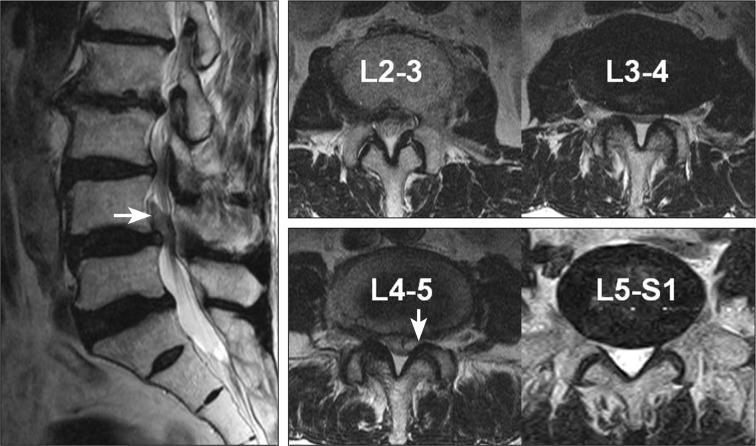
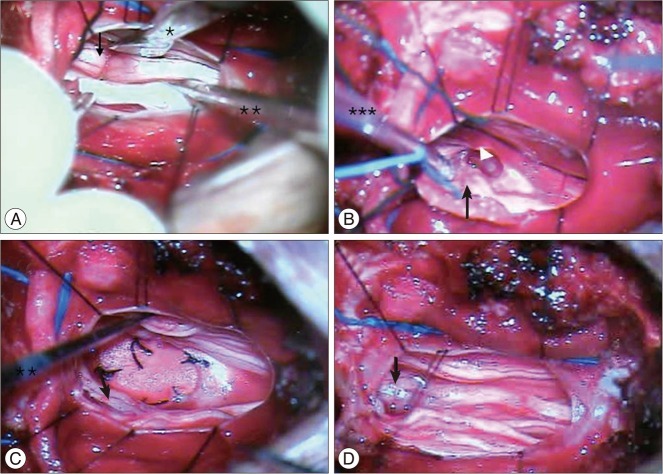
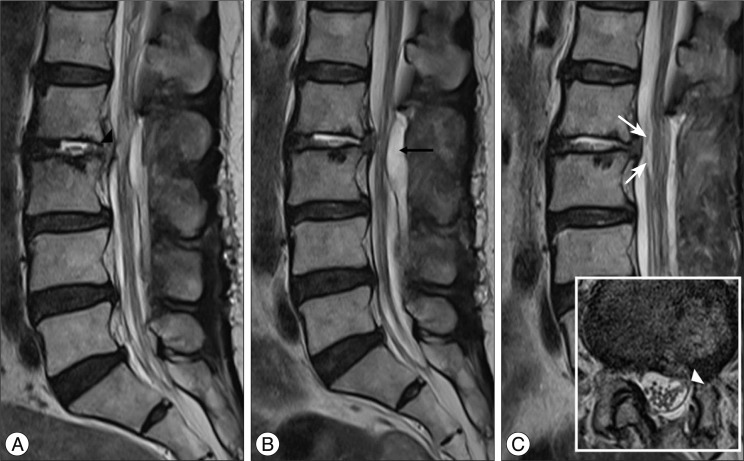
- The authors report 2 cases of nerve root herniation after discectomy of a large lumbar disc herniation caused by an unrecognized dural tear. Patients complained of the abrupt onset of radiating pain after lumbar discectomy. Magnetic resonance imaging showed cerebrospinal fluid signal in the disc space and nerve root displacement into the disc space. Symptoms improved after the herniated nerve root was repositioned. Clinical symptoms and suggestive radiologic image findings are important for early diagnosis and treatment.
Keyword
Figure
Reference
-
1. Ahn Y, Lee HY, Lee SH, Lee JH. Dural tears in percutaneous endoscopic lumbar discectomy. Eur Spine J. 2011; 20:58–64. PMID: 20582555.
Article2. Bosacco SJ, Gardner MJ, Guille JT. Evaluation and treatment of dural tears in lumbar spine surgery : a review. Clin Orthop Relat Res. 2001; 238–247. PMID: 11501817.3. Cammisa FP Jr, Girardi FP, Sangani PK, Parvataneni HK, Cadag S, Sandhu HS. Incidental durotomy in spine surgery. Spine (Phila Pa 1976). 2000; 25:2663–2667. PMID: 11034653.
Article4. Hodges SD, Humphreys SC, Eck JC, Covington LA. Management of incidental durotomy without mandatory bed rest. A retrospective review of 20 cases. Spine (Phila Pa 1976). 1999; 24:2062–2064. PMID: 10528385.5. Jones AA, Stambough JL, Balderston RA, Rothman RH, Booth RE Jr. Long-term results of lumbar spine surgery complicated by unintended incidental durotomy. Spine (Phila Pa 1976). 1989; 14:443–446. PMID: 2718049.
Article6. Nishi S, Hashimoto N, Takagi Y, Tsukahara T. Herniation and entrapment of a nerve root secondary to an unrepaired small dural laceration at lumbar hemilaminectomies. Spine (Phila Pa 1976). 1995; 20:2576–2579. PMID: 8610254.
Article7. Pavlou G, Bucur SD, van Hille PT. Entrapped spinal nerve roots in a pseudomeningocoele as a complication of previous spinal surgery. Acta Neurochir (Wien). 2006; 148:215–219. discussion 219-220. PMID: 16374564.
Article8. Saxler G, Krämer J, Barden B, Kurt A, Pförtner J, Bernsmann K. The long-term clinical sequelae of incidental durotomy in lumbar disc surgery. Spine (Phila Pa 1976). 2005; 30:2298–2302. PMID: 16227893.
Article9. Sin AH, Caldito G, Smith D, Rashidi M, Willis B, Nanda A. Predictive factors for dural tear and cerebrospinal fluid leakage in patients undergoing lumbar surgery. J Neurosurg Spine. 2006; 5:224–227. PMID: 16961083.
Article10. Töppich HG, Feldmann H, Sandvoss G, Meyer F. Intervertebral space nerve root entrapment after lumbar disc surgery. Two cases. Spine (Phila Pa 1976). 1994; 19:249–250. PMID: 8153836.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Conjoined Nerve Root Anomaly Associated with Lumbar Disc Herniation: A Case Report
- A Case of Nerve-Root Anomaly Associated with Herniated Intervertebral Disc in Lumbar: Case Report
- Redundant Nerve Roots of Cauda Equina Mimicking Intradural Disc Herniation: A Case Report
- Spinal Nerve Root Swelling Mimicking Intervertebral Disc Herniation in Magnetic Resonance Imaging: A Case Report
- Minimally Invasive Surgery in Lumbar Disc Herniations with MicroEndoscopic Discectomy System: Technical Note