J Korean Assoc Oral Maxillofac Surg.
2010 Apr;36(2):145-148. 10.5125/jkaoms.2010.36.2.145.
The conservative treatment of mandibular fracture in a child with circummandibular wiring: case report
- Affiliations
-
- 1Department of Dentistry, Oral and Maxillofacial Surgery, Ajou University School of Medicine, Suwon, Korea. arcady@ajou.ac.kr
- KMID: 2190001
- DOI: http://doi.org/10.5125/jkaoms.2010.36.2.145
Abstract
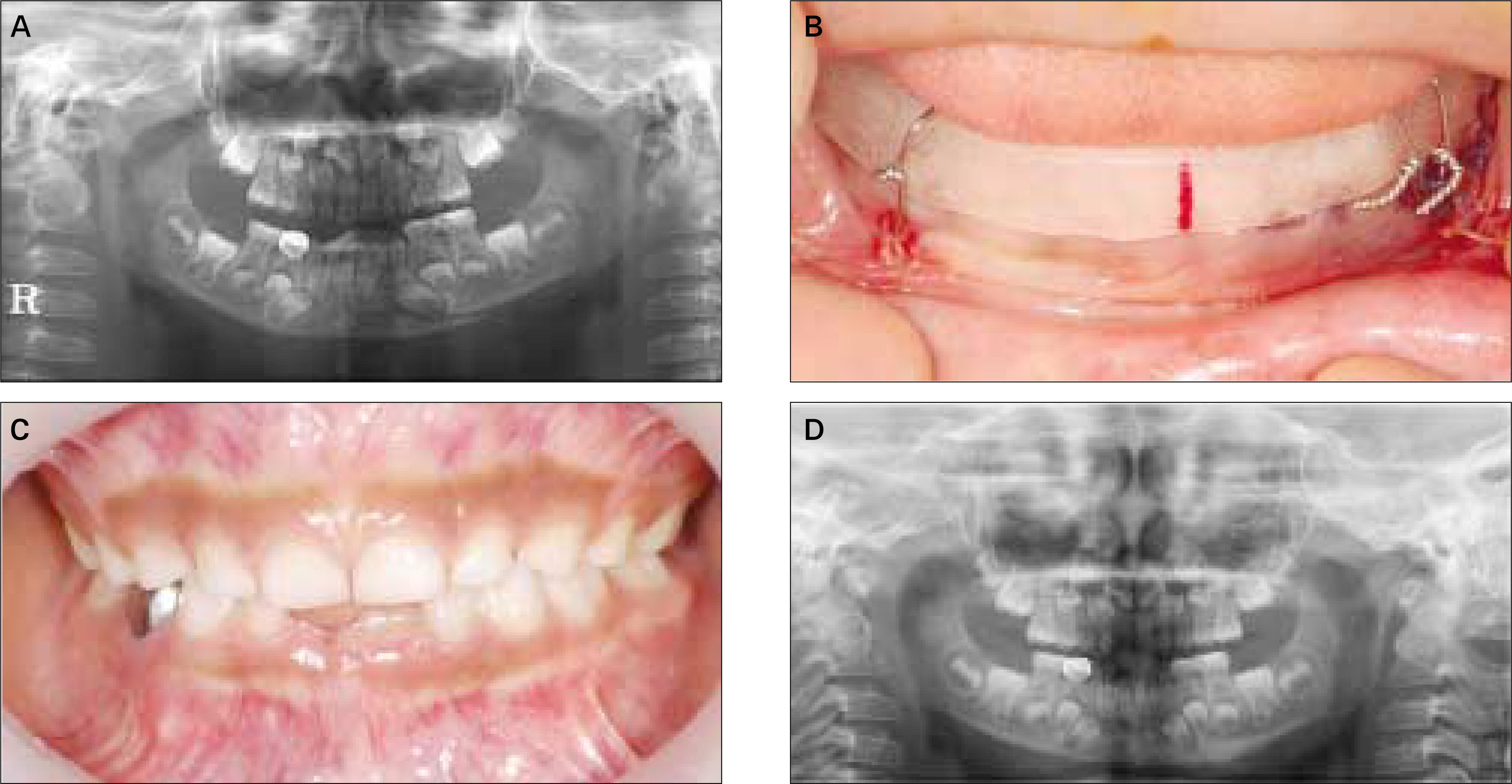
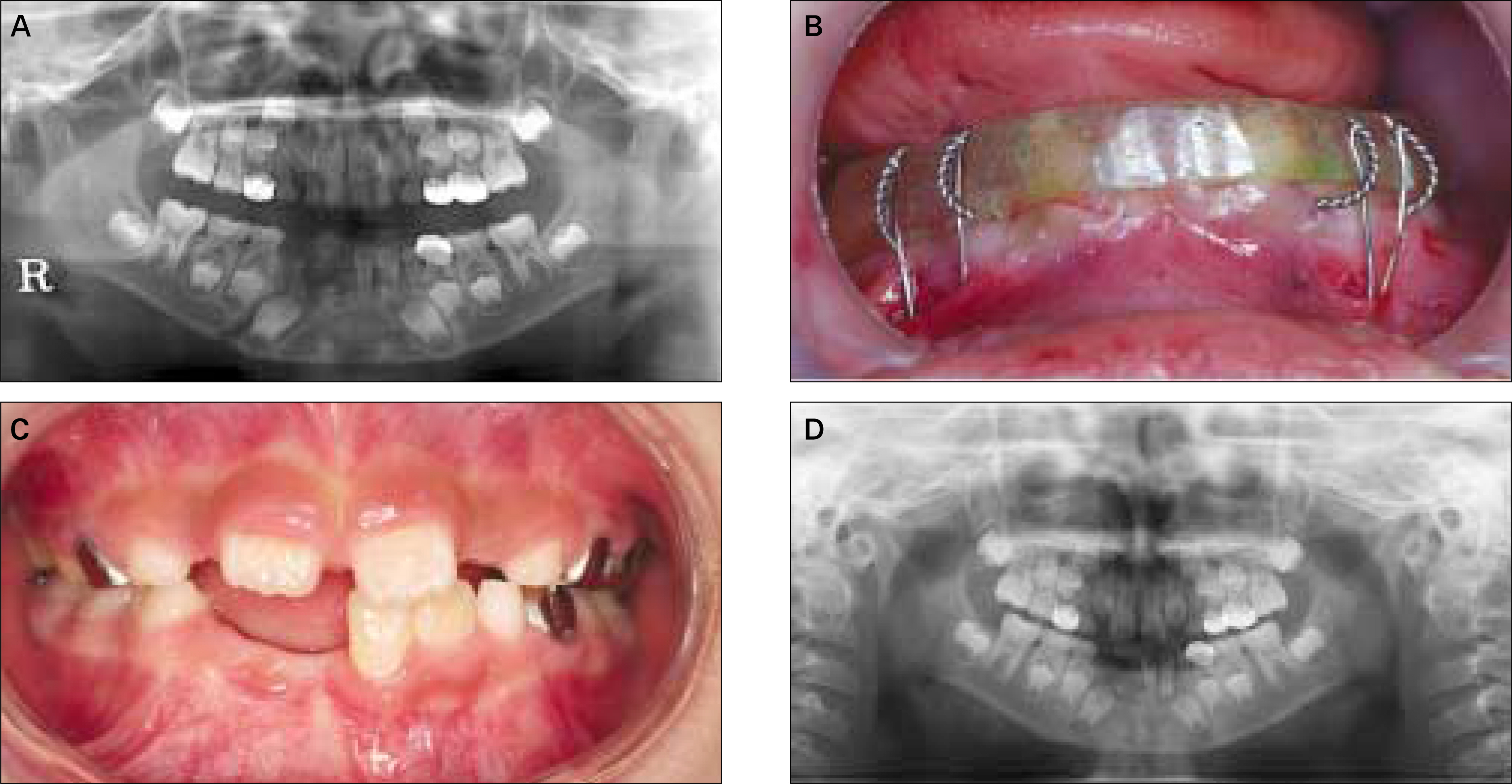
- Maxillofacial injuries are less common in children than in adolescents and adults. This lower incidence is a result of the relatively small size of mandible, the resilient nature of the bones, and a relatively protected environment, which distinguish the treatment principles of pediatric mandibular fractures from those of the adult. The bone of child is malleable, so pediatric fractures tend to be less displaced and rarely comminuted. Moreover, high regeneration potential of the wound allows more conservative treatment modalities for the pediatric mandibular fracture. High risk of damaging unerupted tooth bud renders many clinicians to resort to more conservative treatment modality for the reduction of displaced segments. This case report describes two successful treatment cases using the circummandibular wiring which was applicated to the fracture on parasymphysis of mandible. Circummandibular wiring can protect the tooth buds, and there is no need for intermaxillary fixation so that it prevents the possible complications of intermaxillary fixation such as the temporomandibular joint ankylosis and the facial growth disturbances. The acrylic splint was removed after 3 weeks, which showed clinically good union across the fracture line without complications. They showed complete clinical and radiological bone healing with an optimum occlusion.
MeSH Terms
Figure
Reference
-
References
1. McGraw BL, Cole RR. Pediatric maxillofacial trauma. Age-related variations in injury. Arch Otolaryngol Head Neck Surg. 1990; 116:41–5.
Article2. Iida S, Matsuya T. Paediatiric maxillofacial fractures: their aetio-logical characters and fracture patterns. J Craniomaxillofac Surg. 2002; 30:237–41.3. Qadri GW, Mokhtar SM. Paediatric mandibular fractures: report of a case. Dent Traumatol. 2008; 24:e67–70.
Article4. Imola MJ, Hamlar DD, Shao W, Chowdhury K, Tatum S. Resorbable plate fixation in pediatiric craniofacial surgery: longterm outcome. Arch Facial Plast Surg. 2001; 3:79–90.5. Pyo SW. Circummandibular wirng for pediatric mandibular fracture: case report. J Korean Assoc Oral Maxillofac Surg. 1995; 21:619–26.6. Dodson TB. Mandibular fractures in children. Kelly JP, editor. OMS Knowledge Update, Vol. 1, Part II. Chicago: AAOMS Publishing;1995. p. 95–107.7. Adi M, Ogden GR, Chisholm DM. An analysis of mandibular fractures in Dundee, Scotland (1977 to 1985). Br J Oral Maxillofac Surg. 1990; 28:194–9.
Article8. Lehman JA Jr, Saddawi ND. Fractures of the mandible in children. J Trauma. 1976; 16:773–7.
Article9. Posnick JC, Wells M, Pron GE. Pediatric facial fractures: evolving patterns of treatment. J Oral Maxillofac Surg. 1993; 51:836–44.
Article10. MacLennan WD. Fractures of the mandible in children under the age of six years. Br J Plast Surg. 1956; 9:125–8.11. Gussack GS, Luterman A, Powell RW, Rodgers K, Ramenofsky ML. Pediatric maxillofacial trauma: unique features in diagnosis and treatment. Laryngoscope. 1987; 97:925–30.12. Kaban LB, Troulis MJ. Pediatric oral and maxillofacial surgery. Philadelphia, PA: WB Saunders;2004.13. Anderson PJ. Fractures of the facial skeleton in children. Injury. 1995; 26:47–50.
Article14. Kaban LB, Mulliken JB, Murray JE. Facial fractures in children: an analysis of 122 fractures in 109 patients. Plast Reconstr Surg. 1977; 59:15–20.15. Alexander R, Su JY, Stark MM. An accurate method for open reduction and internal fixation of high and low condylar process fractures. J Oral Maxillofac Surg. 1994; 52:808–12.
Article16. Re′mi M, Christine MC, Gael P, Soizick P, Joseph-Andre′ J. Mandibular fractures in children: long term results. Int J Pediatr Otorhinolaryngol. 2003; 67:25–30.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Open reduction and internal fixation of mandibular fracture in an 11-month-old infant: a case report
- Functional recovery of mandibular high condylar fracture patient with immediate provisional implant: case report
- Tension band wiring and Modified tension band wiring in the Operative Treatment of Patella Fracture
- Clinical study of mandibular fracture of children
- Operative Treatment of patellar Fractures