J Korean Med Assoc.
2009 Nov;52(11):1109-1114. 10.5124/jkma.2009.52.11.1109.
Drug Therapy of Dermatophytosis
- Affiliations
-
- 1Department of Dermatology, Konkuk University College of Medicine, Korea. 20070178@kuh.ac.kr, kjahn@kuh.ac.kr
- KMID: 2188093
- DOI: http://doi.org/10.5124/jkma.2009.52.11.1109
Abstract
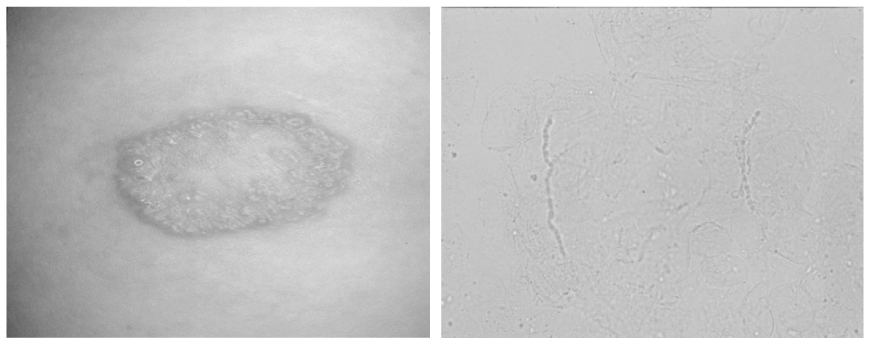
- Dermatophytosis is a superficial infection caused by dermatophytes, a group of taxonomically related fungi. Dematophytes have the ability to form molecular attachments to keratin, use it as a source of nutrients, and then colonize keratinized tissues, including the stratum corneum of the epidermis, hair, nails, and the horny tissues of animals. For an effective treatment of dermatophytosis, antifungal agents must be able to reach dermatophytes in the keratin layer. The concentration of these drugs must also be maintained above therapeutic level for a sustained period of time. Newer oral antifungal agents, itraconazole, terbinafine, and fluconazole are widely used because of the improved therapeutic efficacy and an acceptable adverse effects profile. However, the drugs have different amount of the dose and period of administration, and the interaction of each individual agent is unique in each type of drugs. Therefore, an extreme caution must be exercised during the prescription of these antifungal agents.
Keyword
MeSH Terms
Figure
Reference
-
1. Moon SK, Shin YM, Park SH. Prevalence of tinea pedis and onychomycosis in the aged. Korean J Med Mycol. 2006. 11:132–140.2. Lee SK, Choi JS, Kim KH. A Clinical and mycological study of tinea pedis. Korean J Dermatol. 1995. 33:1029–1037.3. Shannon V, Michael PH, Roderick JH. Superficial and deep fungal infection. Fitapatrick's dermatology In general medicine. 2008. 7th ed. New York: Mc Graw Hill;1807–1831.4. Kim KH, Ahn KJ, Yu HJ. Superficial and deep fungal infection. Dermatology. 2008. 5th ed. Seoul: Yeomoomkak;345–356.5. Kwon KS. The Safety of Antifungal Agents. Korean J Med Mycol. 2001. 6:129–134.6. Amichai Boaz, Grunwald Marcelo H. Adverse drug reactions of the new oral antifungal agents-terbinafine, fluconazole, and itraconazole. Int J Dermatol. 1998. 37:410–415.
Article7. Hall M, Monica C, Krupp P. Safety of oral terbinafine: results of postmarking surveillance study in 25,884 patients. Arch Dermatol. 1997. 133:1213–1219.
Article8. Jacobson MA, Hanks DK, Ferell LD. Fatal acute hepatic necrosis due to fluconazole. Am J Med. 1994. 96:188–190.
Article9. Pursley TJ, Blomquist IK, Abraham J. Fluconazoleinduced congenital anomalies in three infants. Clin Infect Dis. 1996. 22:336–340.
Article10. Park JM, Kwon SJ, Yu HJ. Comparison the growth rate between the affected and the unaffected great toenail in the same patients with onychomycosis. Korean J Med Mycol. 2000. 5:173–178.11. Lee YW, Jeong ST, Ahn KJ. Retrospective study of oral antifungal agents in the treatment of toenail onychomycosis. Korean J Med Mycol. 2002. 7:149–154.12. Hay RJ. The future of onychomycosis therapy may involve a combination of approches. Br J Dermatol. 2001. 145:3–8.
Article13. Baran R, Kaouknov A. Topical antifungal drugs for the treatment of onychomycosis: an overview of current strategies for monotherapy and combination therapy. J Eur Acad Dermatol Venereol. 2005. 19:21–29.
Article14. Kim HC, Jung KB, Shin DH. Comparison of compliance and cure rate of systemic antifungal therapy vs. combination therapy with systemic and topical agent in toenail onychomycosis. Korean J Med Mycol. 2002. 7:35–41.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dermatophytosis: Clinical Manifestation, Diagnosis, and Considerations for Antifungal use
- Mycological Results after Antifungal Treatment of Toenail Dermatophytosis
- Two Cases of Dermatophytosis in Patients with Psoriasis
- Pharmacological Teatment of Tinea Pedis
- The Effect of Oral Ketoconazole in Dermatophytosis