J Korean Med Assoc.
2009 May;52(5):509-517. 10.5124/jkma.2009.52.5.509.
Preoperative Radiological Staging of Rectal Cancer
- Affiliations
-
- 1Department of Radiology, Korea University College of Medicine, Korea. mjkim7@korea.ac.kr
- KMID: 2188018
- DOI: http://doi.org/10.5124/jkma.2009.52.5.509
Abstract
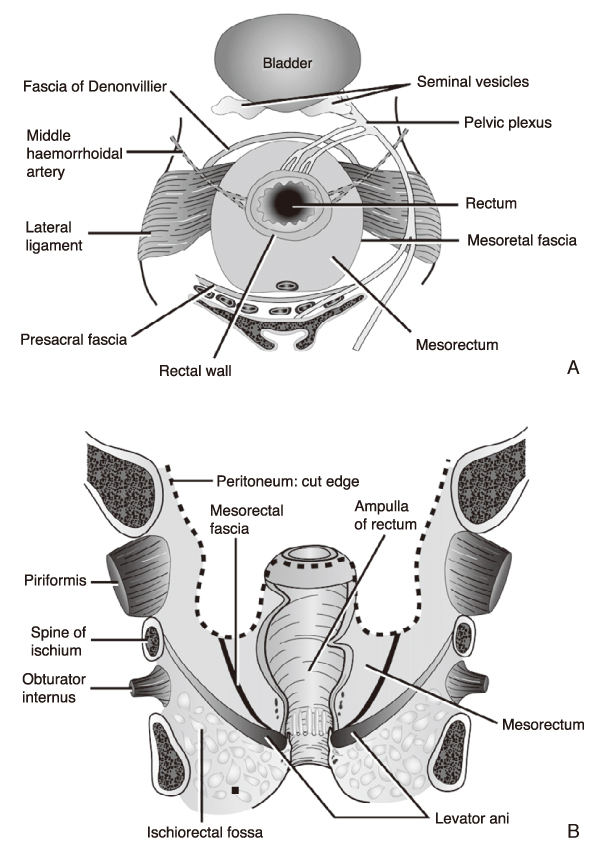
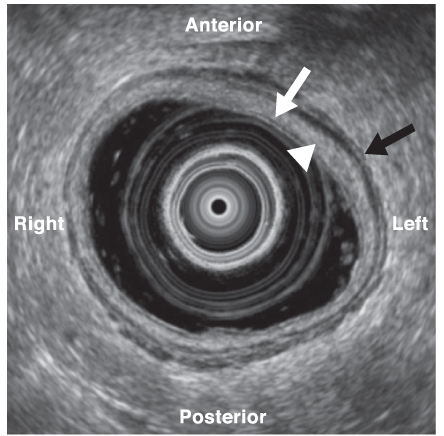
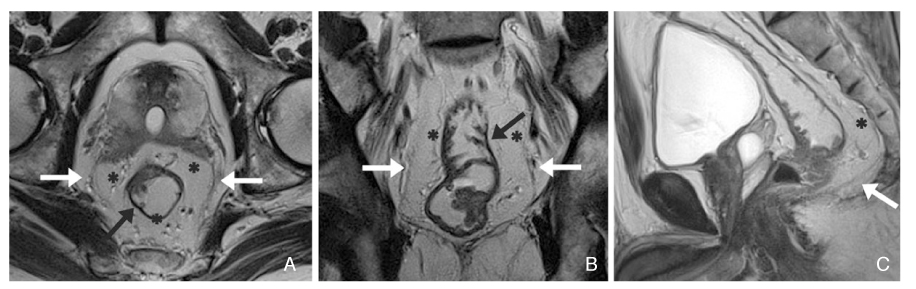
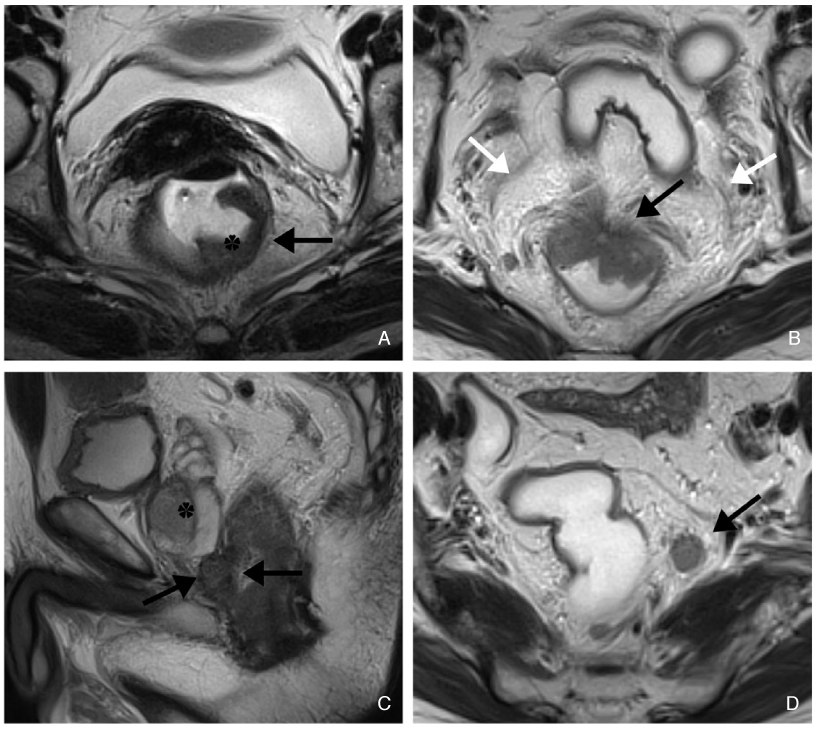
- Rectal cancer is a common malignant disease that continues to have a highly variable outcome, with local recurrence after surgical resection usually leading to an incurable disease. Local recurrence is dependent upon tumor stages and surgical techniques. There is no general consensus on the role of transrectal ultrasonography (TRUS), computed tomography (CT), and magnetic resonance imaging (MRI) in staging of rectal cancer. The role of preoperative imaging is to determine which therapy may be suitable for the patients by surgery alone or with additional treatment. Although the tumor stage is an important prognostic factor, the evaluation of the involvement of the mesorectal fat and mesorectal fascia is even more important. New developments in techniques such as coils, sequences, and gradients in MRI, and evolution of multidetector CT (MDCT) allow better diagnostic options for patients with rectal cancer. Highresolution MRI has proved useful in clarifying the relationship between the tumor and the mesorectal fascia, representing circumferential resection margin at total mesorectal excision. At present, MRI is superior to CT or TRUS for assessing the local staging of rectal cancers. However, nodal staging remains a difficult radiological diagnosis. The role of MDCT has to be set, but for distant metastatic disease it remains to be the first option. This review discusses on the current role of the various imaging modalities in preoperative staging of the rectal cancer.
Keyword
- Rectum; Neoplasm; Ultrasound; CT; MRI
Figure
Reference
-
1. Maier A, Fuchsjager M. Preoperative staging of rectal cancer. Eur J Radiol. 2003. 47:89–97.
Article2. Sung JJ, Lau JY, Goh KL, Leung WK. Increasing incidence of colorectal cancer in Asia: implications for screening. Lancet Oncol. 2005. 6:871–876.
Article3. Quirke P, Durdey P, Dixon MF, Williams NS. Local recurrence of rectal adenocarcinoma due to inadequate surgical resection. Histopathological study of lateral tumour spread and surgical excision. Lancet. 1986. 2:996–999.4. Sagar PM, Pemberton JH. Surgical management of locally recurrent rectal cancer. Br J Surg. 1996. 83:293–304.
Article5. Kapiteijn E, Marijnen CA, Nagtegaal ID, Putter H, Steup WH, Wiggers T, Rutten HJ, Pahlman L, Glimelius B, van Krieken JH, Leer JW, van de Velde CJ. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med. 2001. 345:638–646.
Article6. Goh V, Halligan S, Bartram CI. Local radiological staging of rectal cancer. Clin Radiol. 2004. 59:215–226.
Article7. Beets-Tan RG, Beets GL. Rectal cancer: review with emphasis on MR imaging. Radiology. 2004. 232:335–346.
Article8. Heald RJ, Husband EM, Ryall RD. The mesorectum in rectal cancer surgery-the clue to pelvic recurrence? Br J Surg. 1982. 69:613–616.
Article9. Heald RJ, Ryall RD. Recurrence and survival after total mesorectal excision for rectal cancer. Lancet. 1986. 1:1479–1482.
Article10. Improved survival with preoperative radiotherapy in resectable rectal cancer. Swedish Rectal Cancer Trial. N Engl J Med. 1997. 336:980–987.11. Shank B, Dershaw DD, Caravelli J, Barth J, Enker W. A prospective study of the accuracy of preoperative computed tomographic staging of patients with biopsy-proven rectal carcinoma. Dis Colon Rectum. 1990. 33:285–290.
Article12. Thompson WM, Halvorsen RA, Foster WL Jr, Roberts L, Gibbons R. Preoperative and postoperative CT staging of rectosigmoid carcinoma. AJR Am J Roentgenol. 1986. 146:703–710.
Article13. Filippone A, Ambrosini R, Fuschi M, Marinelli T, Genovesi D, Bonomo L. Preoperative T and N staging of colorectal cancer: accuracy of contrast-enhanced multi-detector row CT colonography-initial experience. Radiology. 2004. 231:83–90.
Article14. Hunerbein M. Endorectal ultrasound in rectal cancer. Colorectal Dis. 2003. 5:402–405.
Article15. Vliegen RF, Beets GL, von Meyenfeldt MF, Kessels AG, Lemaire EE, van Engelshoven JM, Beets-Tan RG. Rectal cancer: MR imaging in local staging--is gadolinium-based contrast material helpful? Radiology. 2005. 234:179–188.
Article16. Schnall MD, Furth EE, Rosato EF, Kressel HY. Rectal tumor stage: correlation of endorectal MR imaging and pathologic findings. Radiology. 1994. 190:709–714.
Article17. Brown G, Richards CJ, Newcombe RG, Dallimore NS, Radcliffe AG, Carey DP, Bourne MW, Williams GT. Rectal carcinoma: thin-section MR imaging for staging in 28 patients. Radiology. 1999. 211:215–222.
Article18. Beets-Tan RG, Beets GL, Vliegen RF, Kessels AG, Van Boven H, De Bruine A, von Meyenfeldt MF, Baeten CG, van Engelshoven JM. Accuracy of magnetic resonance imaging in prediction of tumour-free resection margin in rectal cancer surgery. Lancet. 2001. 357:497–504.
Article19. Iafrate F, Laghi A, Paolantonio P, Rengo M, Mercantini P, Ferri M, Ziparo V, Passariello R. Preoperative staging of rectal cancer with MR Imaging: correlation with surgical and histopathologic findings. Radiographics. 2006. 26:701–714.
Article20. Kim JH, Beets GL, Kim MJ, Kessels AG, Beets-Tan RG. High-resolution MR imaging for nodal staging in rectal cancer: are there any criteria in addition to the size. Eur J Radiol. 2004. 52:78–83.
Article21. Dworak O. Number and size of lymph nodes and node metastases in rectal carcinomas. Surg Endosc. 1989. 3:96–99.
Article22. Monig SP, Baldus SE, Zirbes TK, Schroder W, Lindemann DG, Dienes HP, Holscher AH. Lymph node size and metastatic infiltration in colon cancer. Ann Surg Oncol. 1999. 6:579.
Article23. de Haas-Kock DF, Baeten CG, Jager JJ, Langendijk JA, Schouten LJ, Volovics A, Arends JW. Prognostic significance of radial margins of clearance in rectal cancer. Br J Surg. 1996. 83:781–785.
Article24. Kwok H, Bissett IP, Hill GL. Preoperative staging of rectal cancer. Int J Colorectal Dis. 2000. 15:9–20.
Article25. Balthazar EJ, Megibow AJ, Hulnick D, Naidich DP. Carcinoma of the colon: detection and preoperative staging by CT. AJR Am J Roentgenol. 1988. 150:301–301.
Article26. Rifkin MD, Ehrlich SM, Marks G. Staging of rectal carcinoma: prospective comparison of endorectal US and CT. Radiology. 1989. 170:319.
Article27. Brown G, Richards CJ, Bourne MW, Newcombe RG, Radcliffe AG, Dallimore NS, Williams GT. Morphologic predictors of lymph node status in rectal cancer with use of high-spatial-resolution MR imaging with histopathologic comparison. Radiology. 2003. 227:371–377.
Article28. Koh DM, Brown G, Temple L, Raja A, Toomey P, Bett N, Norman AR, Husband JE. Rectal cancer: mesorectal lymph nodes at MR imaging with USPIO versus histopathologic findings-initial observations. Radiology. 2004. 231:91–99.
Article29. Schoemaker D, Black R, Giles L, Toouli J. Yearly colonoscopy, liver CT, and chest radiography do not influence 5-year survival of colorectal cancer patients. Gastroenterology. 1998. 114:7–14.
Article30. Leen E, Angerson WJ, Wotherspoon H, Moule B, Cook TG, McArdle CS. Detection of colorectal liver metastases: comparison of laparotomy, CT, US, and Doppler perfusion index and evaluation of postoperative follow-up results. Radiology. 1995. 195:113–116.
Article31. Kim YK, Ko SW, Hwang SB, Kim CS, Yu HC. Detection and characterization of liver metastases: 16-slice multidetector computed tomography versus superparamagnetic iron oxideenhanced magnetic resonance imaging. Eur Radiol. 2006. 16:1337–1345.
Article32. Karantanas AH, Yarmenitis S, Papanikolaou N, Gourtsoyiannis N. Preoperative imaging staging of rectal cancer. Dig Dis. 2007. 25:20–32.
Article33. Bipat S, Glas AS, Slors FJ, Zwinderman AH, Bossuyt PM, Stoker J. Rectal cancer: local staging and assessment of lymph node involvement with endoluminal US, CT, and MR imaging--a meta-analysis. Radiology. 2004. 232:773–783.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Preoperative Staging of Rectal Cancer by CT & MRI
- TNM Staging, Molecular Staging and Prognostic Factors of Rectal Cancer
- Clinical Significance of Preoperative Magnetic Resonance Imaging in Staging of Rectal Cancer
- Transrectal ultrasonography in preoperative staging of rectal cancer
- Usefulness of hydrocolonic sonograpy in the staging of colorectal cancer