J Korean Orthop Assoc.
2009 Feb;44(1):145-150. 10.4055/jkoa.2009.44.1.145.
Delayed Diagnosis of Acute Hematogenous Osteomyelitis of the Acetabulum: Report of Two Cases
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Soonchunhyang University, Cheonan, Korea. awe@korea.com
- KMID: 2186391
- DOI: http://doi.org/10.4055/jkoa.2009.44.1.145
Abstract
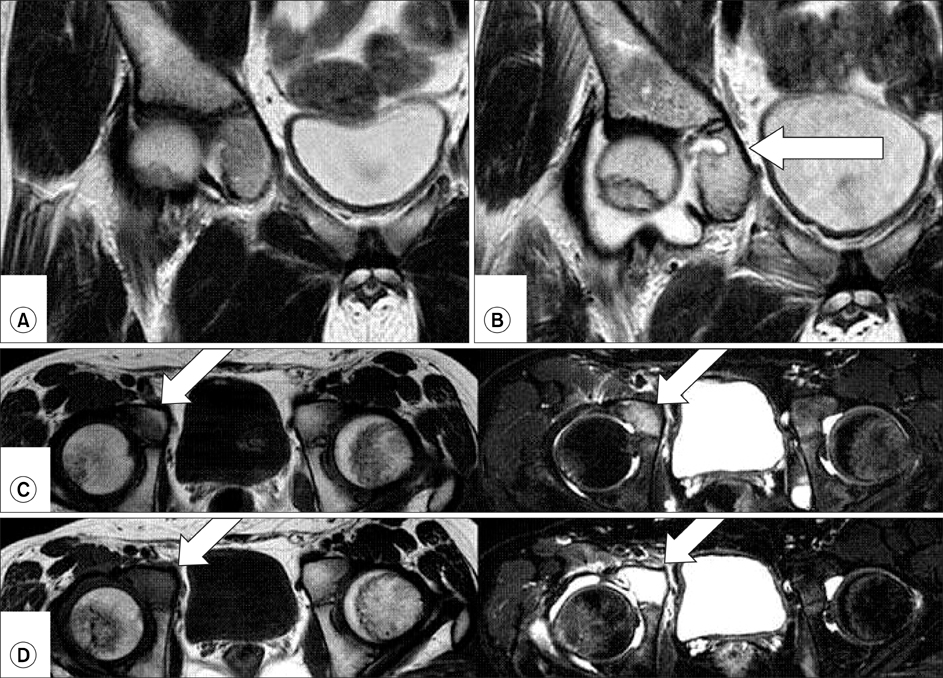
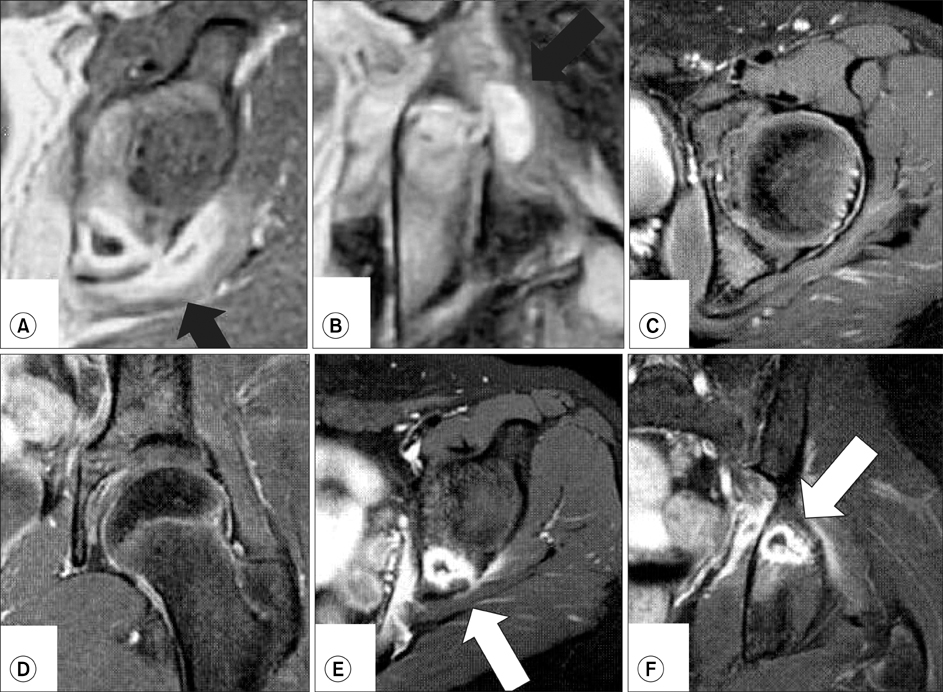
- Acute hematogenous osteomyelitis of the acetabulum is not a common disease with similar clinical symptoms and hematological findings to those of pyogenic arthritis of the hip joint. This symptom similarity might lead to a delayed diagnosis of the disease, and even to unnecessary surgery. We report two cases of acute hematogenous osteomyelitis of the acetabulum. One was a 13-year-old boy with non-specific radiological findings of the hip joint, who was initially diagnosed with fever of unknown origin. The other was an 11-year-old boy with hip joint pain and a recent history of minor trauma, which lead to a delayed diagnosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Davidson D, Letts M, Khoshhal K. Pelvic osteomyelitis in children: a comparison of decades from 1980-1989 with 1990-2001. J Pediatr Orthop. 2003. 23:514–521.2. De Boeck H, Haentjens P, Verhaven E. Osteomyelitis of the actabulum. Acta Orthop Belg. 1990. 56:621–623.3. Edwards MS, Baker CJ, Granberry WM, Barrett FF. Pelvic osteomyelitis in children. Pediatrics. 1978. 61:62–67.4. Gamble JG, Rinsky LA, Bleck EE. Acetabular osteomyelitis in children. Clin Orthop Relat Res. 1984. 186:71–74.5. Highland TR, LaMont RL. Osteomyelitis of the pelvis in children. J Bone Joint Surg Am. 1983. 65:230–234.6. Klein JD, Leach KA. Pediatric pelvic osteomyelitis. Clin Pediatr (Phila). 2007. 46:787–790.7. Rand N, Mosheiff R, Matan Y, Porat S, Shapiro M, Liebergall M. Osteomyelitis of the pelvis. J Bone Joint Surg Br. 1993. 75:731–733.8. Suk SI, Lee CK, Ahn JK, et al. Orthopaedics. 2006. 6th ed. Seoul: Newest medical publishing company;272–274.9. Weber-Chrysochoou C, Corti N, Goetschel P, Altermatt S, Huisman TA, Berger C. Pelvic osteomyelitis: a diagnostic challenge in children. J Pediatr Surg. 2007. 42:553–557.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Observation of Hematogenous Osteomyelitis of Fibula in Children
- Diagnosis of Osteomyelitis by the Sequential Use of â¹â¹mTc - Methylene Diphosphonate and â¶â·Ga Imaging
- Hematogenous Osteomyelitis Occurred in Adult Long Bones
- Clinical Observation of Acute Hematogenous Osteomyelitis in Children
- A Clinical Study on Hematogenous Osteomyelitis in Children