J Korean Orthop Assoc.
2009 Feb;44(1):1-7. 10.4055/jkoa.2009.44.1.1.
Comparison with Number and Position of Percutaneous Iliosacral Screws as Treatment of Unstable Pelvic Fracture
- Affiliations
-
- 1Department of Orthopedic Surgery, Daejeon St. Mary's Hospital, The Catholic University of Korea College of Medicine, Daejeon, Korea. osmcy@naver.com
- KMID: 2186371
- DOI: http://doi.org/10.4055/jkoa.2009.44.1.1
Abstract
-
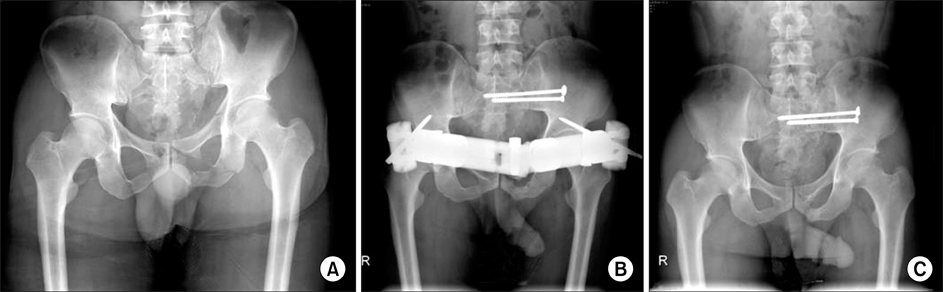
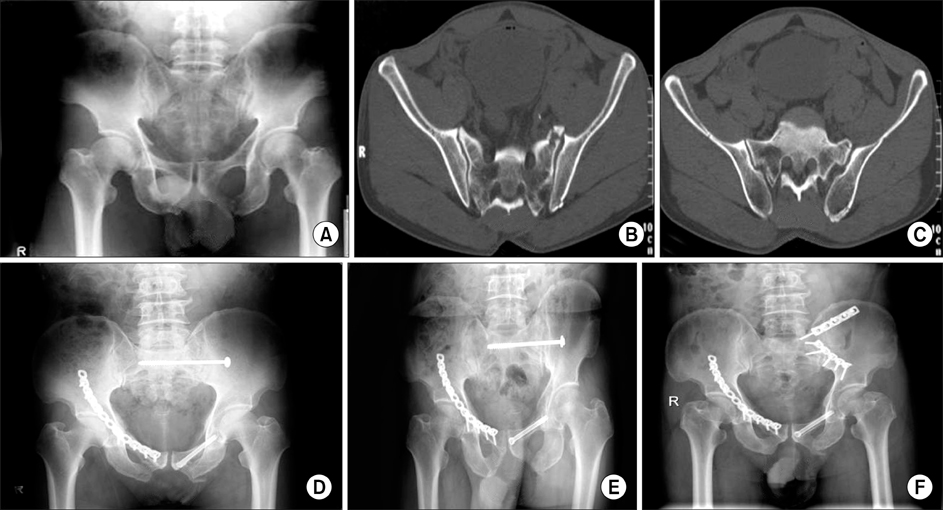
PURPOSE: A closed reduction of the posterior arch and percutaneous fixation with S1 and S2 iliosacral (IS) screw was performed on an unstable pelvis fracture with a disruption of the sacroiliac complex. The radiological and clinical results were analyzed according the number of screws and their position.
MATERIALS AND METHODS
Of 31 cases with an unstable pelvis fracture involving the sacral complex, classified as Tile type C (AO/OTA), 16 and 15 cases were treated with one S1 screw fixation and two screws fixation into S1 and S2, respectively, using a percutaneous fixation technique. The patients were followed up for a minimum of 12 months and the radiological and clinical outcomes were analyzed statistically using the Majeed score and SF-36.
RESULTS
Five cases of screw displacement occurred in the one screw fixation group. On the other hand, there was no screw displacement in the two screws fixation group after a mean follow-up of 40.2 months. In the case of a narrow safe zone (iliac cortical density, ICD), it is impossible to fix with two S1 screws. However, in these patients, good clinical results were achieved with S1 and S2 were achieved with S1 and S2 screw without complications.
CONCLUSION
The technique of two screws fixation is an efficient and reliable method for reducing and fixing the unstable pelvic ring disruptions. Additional S2 screw fixation is recommended for patients with a narrow ICD.
Keyword
Figure
Cited by 2 articles
-
Operative Treatment of Unstable Pelvic Ring Injury
Sang Hong Lee, Sang Ho Ha, Young Kwan Lee, Sung Won Cho, Sang Soo Park
J Korean Fract Soc. 2012;25(4):243-249. doi: 10.12671/jkfs.2012.25.4.243.Operative Treatment of Unstable Pelvic Ring Injury
Sang Hong Lee, Sang Ho Ha, Young Kwan Lee, Sung Won Cho, Sang Soo Park
J Korean Fract Soc. 2012;25(4):243-249. doi: 10.12671/jkfs.2012.25.4.243.
Reference
-
1. Bucholz RW. The pathological anatomy of Malgaine fracture-dislocation of the pelvis. J Bone joint Surg Am. 1981. 63:400–404.2. Diliberti T, Reardon J, Lindsey R. The optimal radiographic intraoperative assessment in the placement of sacroiliac joint screws. Orthop Trans. 1993-1994. 17:1190.3. Dujardin FH, Roussignol X, Hossembaccus M, Thomine JM. Experimental study of the sacroiliac joint micromotion in pelvic disruption. J Orthop Trauma. 2002. 16:99–103.
Article4. Ebraheim N, Rusin J, Coombs R, Jackson WT, Holiday B. Percutaneous computer tomography-stabilization of pelvic fracture: preliminary report. J Orthop Trauma. 1987. 1:197–204.5. Goldstein A, Phillips T, Selafani SJ, et al. Early open reduction and internal fixation of the disrupted pelvic ring. J Trauma. 1986. 26:325–333.6. Hoffmann E, Lenoir T, Morel E, Levassor N, Rillardon L, Guigui P. Posterior bridging osteosynthesis for traumatic sacroiliac joint dislocation: a report of seven cases. Eur J Orthop Surg Traumatol. 2008. 18:47–53.
Article7. Keating JF, Werier MC, Blacht P, et al. Early fixation of the vertically unstable pelvis: the role of iliosacral screw fixation of the posterior lesion. J Orthop Trauma. 1999. 13:107–113.
Article8. Kellam JF, McMurtry RY, Paley D, Tile M. The unstable pelvic fracture. Operative treatment. Orthop Clin North Am. 1987. 18:25–41.9. Kim JJ, Kim JW, Chang JS. Clinical outcome of AO type C pelvic ring injury. J Korean Orhtop Assoc. 2005. 40:181–187.
Article10. Kim WY, Hearn TC, Seleem O, Mahalingam E, Stephen D, Tile M. Effect of pin location on stability of pelvic external fixation. Clin Orthop Relat Res. 1999. 361:237–244.
Article11. Kim WY, Ji JH, Kim YY, Yang YJ, Lee DY. Anterior fixation techniques on unstable pelvic ring injury. J Korean Assoc. 2005. 40:8–13.
Article12. Majeed SA. Grading the outcome of plevic fractures. J Bone Joint Surg Br. 1989. 71:304–306.13. Matta JM, Saucedo T. Internal fixation of pelvic ring fractures. Clin Orthop Relat Res. 1989. 242:83–97.
Article14. McLaren AC, Rorabeck CH, Halpeeny J. Long-term pain and disability in relation to residual deformity after displaced pelvic ring fractures. Can J Surg. 1990. 33:492–494.15. Mowed BR, Geer BL. S2 Iliosacral screw fixation for disruption of the posterior pelvic ring: a report of 49 cases. J Orhtop Trauma. 2006. 20:378–383.16. Mullis BH, Sagi HC. Minimum 1-year follow-up for patients with vertical shear sacroiliac joint dislocations treated either iliosacral screws: does joint ankylosis of anatomic reduction contribute to functional outcome? J Orthop Trauma. 2008. 22:293–298.17. Oliver CW, Twaddle B, Agel J, Routt ML Jr. Outcome after pelvic ring fractures: evaluation using the medical outcomes short from SF-36. Injury. 1996. 27:635–641.18. Pohlemann T, Gänsslen A, Schelwald O, Culemann U, Tscherne H. Outcome after pelvic ring injuries. Injury. 1996. 27:Suppl 2. B31–B38.
Article19. Routt ML Jr, Kregor PJ, Simonian PT, Mayo KA. Early results of percutaneous Iliosacral screws placed with the patient in the supine position. J Orthop Trauma. 1995. 9:207–214.20. Routt ML Jr, Meier MC, Kregor PJ, Mayo KA. Percutaneous iliosacral screws with the patient's supine technique. Oper Tech Orthop. 1993. 3:35–45.21. Routt ML Jr, Simonian PT, Mills WJ. Iliosacral screw fixation: early complications of the percutaneous technique. J Orthop Trauma. 1997. 11:584–589.22. Rubash HE, Brown TD, Nelson DD, Mears DC. Comparative mechanical performances of some new devices for fixation of unstable pelvic fractures. Med Biol Eng Comput. 1983. 21:657–663.23. Shuler T, Boone D, Gruen G, Peitzman A. Percutaneous iliosacral screw fixation: early treatment for unstable posterior pelvic ring disruptions. J Trauma. 1995. 38:453–458.24. Simpson LA, Waddell JP, Leighton PK, Kellam JF, Tile M. Anterior approach and stabilization of the disrupted sacroiliac joint. J Trauma. 1987. 27:1332–1339.
Article25. Templeman D, Goulet J, Duwelius PJ, Olson S, Davidson M. Internal fixation of displaced fractures of the sacrum. Clin Orthop Relat Res. 1996. 329:180–185.
Article26. Tile M. Pelvic ring fractures: should they be fixed? J Bone Joint Surg Br. 1988. 70:1–12.
Article27. van den Bosch EW, van Zwienen CM, van Vugt AB. Fluoroscopic positioning of sacroiliac screws in 88 patients. J Trauma. 2002. 53:44–48.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous Iliosacral Screw Fixation in Unstable Pelvic Ring Injury
- Superior Gluteal Artery Injury during Percutaneous Iliosacral Screw Fixation: A Case Report
- Percutaneous Iliosacral Screw Fixation for Pelvic Ring Injury
- Iliosacral Screw Fixation of the Posterior Pelvic Ring Using Local Anesthesia and Computerized Tomography
- Treatment of Unstable Sacral Fractures Related to Spino-Pelvic Dissociations