J Korean Orthop Assoc.
2009 Dec;44(6):680-685. 10.4055/jkoa.2009.44.6.680.
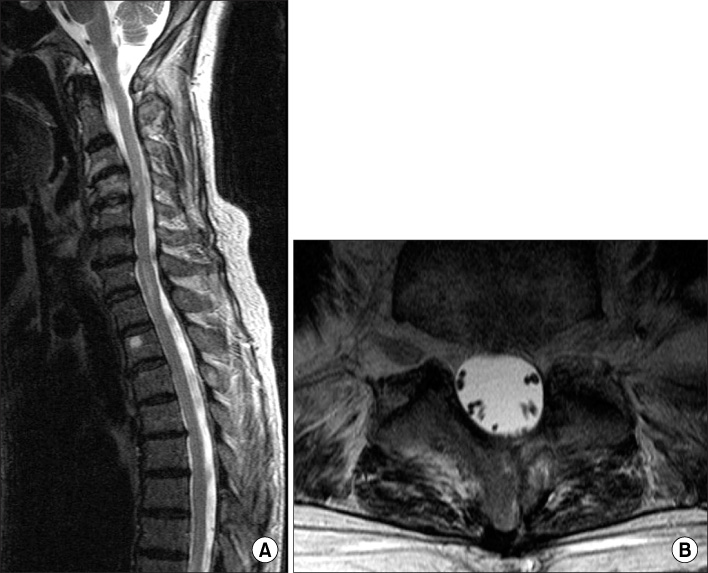
Unusual Spinal Epidural Abscess without Predisposing Factors Treated Using a Minimally Invasive Technique
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Research Institute of Clinical Medicine, Chonbuk National University, Jeonju, Korea.
- 2Department of Orthopedic Surgery, Gwangju Veterans Hospital, Gwangju, Korea. alla1013@naver.com
- KMID: 2186296
- DOI: http://doi.org/10.4055/jkoa.2009.44.6.680
Abstract
- Spinal epidural abscess (SEA) is an uncommon infectious disease that can have disastrous neurologic complications. Previous reports have identified underlying predisposing characteristics. Here, the authors report unusual 2 cases of multi-segment spinal epidural abscess, without predisposing conditions, which were successfully treated using a minimally invasive technique.
MeSH Terms
Figure
Reference
-
1. Baker AS, Ojeman RG, Swartz MN, Richardson EP Jr. Spinal epidural abscess. N Engl J Med. 1975. 293:463–468.
Article2. Danner RL, Hartman BJ. Update of spinal epidural abscess: 35 cases and review of the literature. Rev Infect Dis. 1987. 9:265–274.
Article3. Ptaszynski AE, Hooten WM, Huntoon MA. The incidence of spontaneous epidural abscess in Olmsted County from 1990 through 2000: a rare cause of spinal pain. Pain Med. 2007. 8:338–343.
Article4. Schultz KD Jr, Comey CH, Haid RW Jr. Technical note. Pyogenic spinal epidural abscess: a minimally invasive technique for multisegmental decompression. J Spinal Disord. 2001. 14:546–549.5. Lyu RK, Chen CJ, Tang LM, Chen ST. Spinal epidural abscess successfully treated with percutaneous, computed tomography-guided, needle aspiration and parenteral antibiotic therapy: case report and review of the literature. Neurosurgery. 2002. 51:509–512.
Article6. Choi CH, Kim HJ, Pai HJ, Park YS. Cervical and thoracolumbar epidural abscess: a case report. J Korean Soc Spine Surg. 2007. 14:105–109.7. Reihsaus E, Waldbaur H, Seeling W. Spinal epidural abscess: a meta-analysis of 915 patients. Neurosurg Rev. 2000. 23:175–204.
Article8. Wheeler D, Keiser P, Rigamonti D, Keay S. Medical management of spinal epidural abscesses: case report and review. Clin Infect Dis. 1992. 15:22–27.
Article9. Panagiotopoulos V, Konstantinou D, Solomou E, Panagiotopoulos E, Marangos M, Maraziotis T. Extended cervicolumbar spinal epidural abscess associated with paraparesis successfully decompressed using a minimally invasive technique. Spine (Phila Pa 1976). 2004. 29:E300–E303.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Irrigation for Lumbar Spinal Epidural Abscess using a Trans-Sacral Epiduroscopic Laser Decompression Catheter
- Extensive Spinal Epidural Abscess: The Usefulness of Minimal Invasive Surgical Technique using Epidural Irrigation Catheter
- Minimally Invasive Surgical Treatment of the Pan-Spinal Anterior Epidural Abscess Using a Nasogastric Tube and Guide Wire
- Transforaminal Endoscopic Drainage of Massive Anterior Epidural Abscess-Novel Technique
- Chronic Spinal Epidural Abscess after Epidural Analgesia: Case Report