J Korean Orthop Assoc.
2011 Aug;46(4):288-293. 10.4055/jkoa.2011.46.4.288.
Efficacy of Interscalene Block Anesthesia on the Early Postoperative Pain after Arthroscopic Shoulder Surgery: Comparison with General Anesthesia
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Chungbuk National University, Cheongju, Korea. oslion@chungbuk.ac.kr
- 2Department of Anesthesiology and Pain Medicine, College of Medicine, Chungbuk National University, Cheongju, Korea.
- KMID: 2185426
- DOI: http://doi.org/10.4055/jkoa.2011.46.4.288
Abstract
- PURPOSE
After shoulder arthroscopy via general anesthesia, most patients complain of severe pain during the early post operative period. In this study, the efficacy of pain control during the early post operative period with interscalene block anesthesia for shoulder arthroscopy was investigated and compared with general anesthesia.
MATERIALS AND METHODS
A prospective randomized controlled study was conducted on 40 patients who underwent shoulder arthroscopy between September 2008 and March 2009. The patients were grouped according to the method of anesthesia. The visual analogue scale (VAS) at the preoperative and early postoperative periods was checked and compared. In addition, the duration of patient controlled analgesia (PCA) usage and additional pain killer injections were examined.
RESULTS
There was no significant difference between the two groups for the VAS score before surgery, but the interscalene block group showed a significantly lower VAS score. The duration of PCA usage was also significantly longer for the interscalene block group, which implies less pain. The number of additional pain killer injections was significantly less in the interscalene block group.
CONCLUSION
The patients who underwent shoulder arthroscopy with interscalene block had significantly less pain during the immediately post operative period for up to 48 hours. So patients could conduct initial rehabilitation and experience minimized side effects caused by analgesics due to the decreased use of pain killer. Therefore, interscalene block is considered a good method of anesthesia for the immediate postoperative pain control after shoulder arthroscopy.
MeSH Terms
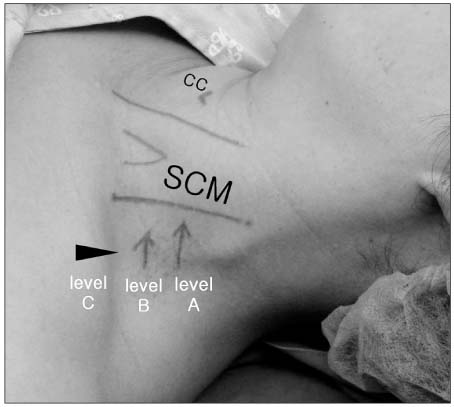
Figure
Reference
-
1. Ramsey ML, Getz CL, Parsons BO. What's new in shoulder and elbow surgery. J Bone Joint Surg Am. 2009. 91:1283–1293.
Article2. Seo JB, Bahng SC. Early complications after repair of massive rotator cuff tear. J Korean Shoulder Elbow Soc. 2006. 9:27–33.
Article3. Oh JH, Kim WS, Kim JY, et al. Continuous intra-lesional infusion combined with interscalene block for effective postoperative analgesia after arthroscopic shoulder surgery. J Korean Shoulder Elbow Soc. 2005. 8:141–147.
Article4. Brown AR, Weiss R, Greenberg C, Flatow EL, Bigliani LU. Interscalene block for shoulder arthroscopy: comparison with general anesthesia. Arthroscopy. 1993. 9:295–300.
Article5. Webb D, Guttmann D, Cawley P, Lubowitz JH. Continuous infusion of a local anesthetic versus interscalene block for postoperative pain control after arthroscopic shoulder surgery. Arthroscopy. 2007. 23:1006–1011.
Article6. Trompeter A, Camilleri G, Narang K, Hauf W, Venn R. Analgesia requirements after interscalene block for shoulder arthroscopy: the 5 days following surgery. Arch Orthop Trauma Surg. 2010. 130:417–421.7. Perlas A, Chan VWS. Ultrasound guided interscalene brachial plexus block. Tech Reg Anesth Pain Manag. 2004. 8:143–148.8. Karkabi S, Besser M, Zinman C. Arthroscopic subacromial decompression performed under local anesthesia. Arthroscopy. 2005. 21:1404.
Article9. Bishop JY, Sprague M, Gelber J, et al. Interscalene regional anesthesia for shoulder surgery. J Bone Joint Surg Am. 2005. 87:974–979.
Article10. Ciccone WJ 2nd, Busey TD, Weinstein DM, Walden DL, Elias JJ. Assessment of pain relief provided by interscalene regional block and infusion pump after arthroscopic shoulder surgery. Arthroscopy. 2008. 24:14–19.
Article11. Goebel S, Stehle J, Schwemmer U, Reppenhagen S, Rath B, Gohlke F. Interscalene brachial plexus block for open-shoulder surgery: a randomized, double-blind, placebo-controlled trial between single-shot anesthesia and patient-controlled catheter system. Arch Orthop Trauma Surg. 2010. 130:533–540.
Article12. Weber SC, Jain R. Scalene regional anesthesia for shoulder surgery in a community setting: an assessment of risk. J Bone Joint Surg Am. 2002. 84:775–779.13. Brull R, McCartney CJL, Sawyer RJ, von Schroeder HP. The indications and applications of interscalene brachial plexus block for surgery about the shoulder. Acute Pain. 2004. 6:57–77.
Article14. Arciero RA, Taylor DC, Harrison SA, Snyder RJ, Leahy KE, Uhorchak JM. Interscalene anesthesia for shoulder arthroscopy in a community-sized military hospital. Arthroscopy. 1996. 12:715–719.
Article15. Flowers GA, Meyers JF. Pseudoaneurysm after interscalene block for a rotator cuff repair. Arthroscopy. 2004. 20:Suppl 2. 67–69.
Article16. Burdine JM, Brown AR, Levine WN, Weber SC, Jain R. Complication rates of scalene regional anesthesia. J Bone Joint Surg Am. 2002. 84-A:1891.
Article17. McCracken LM, Keogh E. Acceptance, mindfulness, and values-based action may counteract fear and avoidance of emotions in chronic pain: an analysis of anxiety sensitivity. J Pain. 2009. 10:408–415.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The effect of sono-guided brachial plexus block on postoperative pain control for arthroscopic shoulder surgery: comparison with general anesthesia
- Interscalene Brachial Plexus Block Following Suprascapular Nerve Block for Humeral Head Surgery in a Patient with Difficult Supine Position: A case report
- The Effect of Preoperative Interscalene Block Using Low-Dose Mepivacaine on the Postoperative Pain after Shoulder Arthroscopic Surgery
- Regional nerve blocks for relieving postoperative pain in arthroscopic rotator cuff repair
- The effect of interscalene brachial plexus block with propofol sedation on preventing perioperative hypothermia during arthroscopic shoulder surgery