J Korean Orthop Assoc.
2011 Aug;46(4):282-287. 10.4055/jkoa.2011.46.4.282.
Comparison of Ultrasonography and MRI in Measuring of Cervical Soft Tissue Structure
- Affiliations
-
- 1Department of Orthopaedic Surgery, School of Medicine, Wonkwang University, Iksan, Korea. osktg@wonkwang.ac.kr
- KMID: 2185425
- DOI: http://doi.org/10.4055/jkoa.2011.46.4.282
Abstract
- PURPOSE
We wanted to determine the usefullness of ultrasonography for exploring cervical anatomical structures and to compare its results with those of magnetic resonance imaging.
MATERIALS AND METHODS
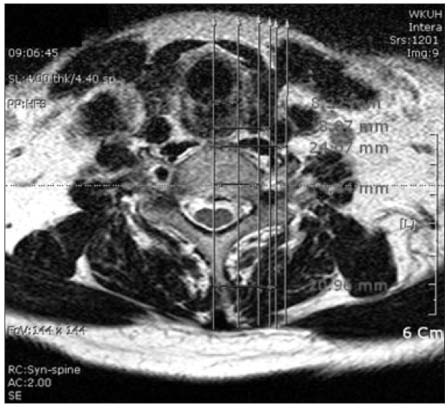
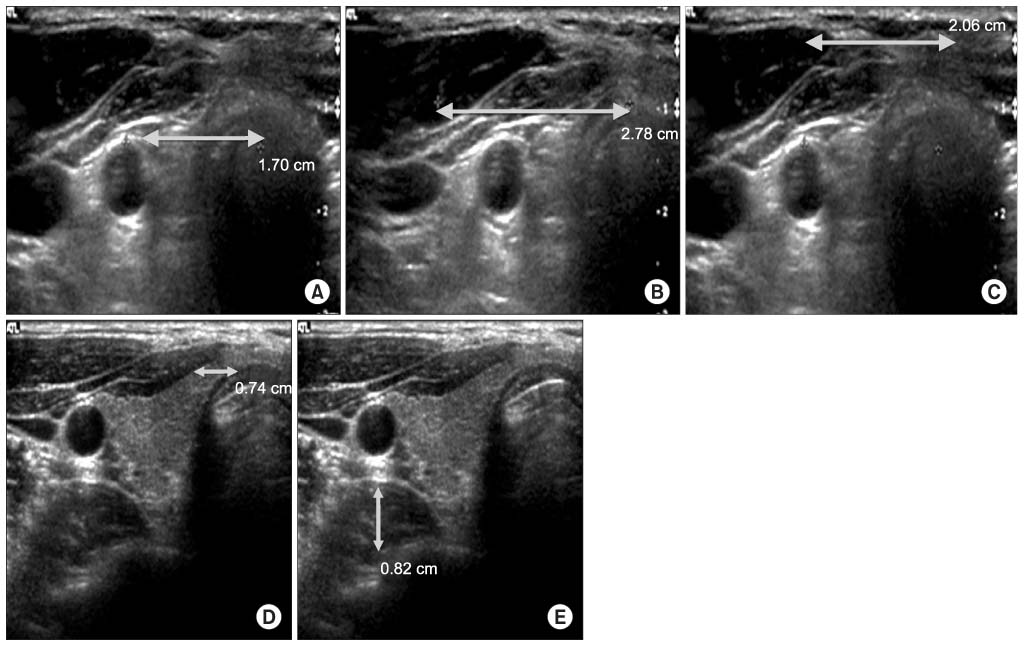
Between May, 2008 and January, 2009, 16 patient (8 male patients and 8 female patients, average age: 55.5 years old) with neck pain following in out patient clinic and who had cervical MRI performed were selected. By using ultrasonography, we measured the shortest distance of the internal carotid artery, internal jugular vein, sternocleidomastoid muscle and longus colli muscle based on the vertebral body of cricoid cartilage. We also measured the thickness of the longus colli muscle. We measured the average length of the shortest distance and thickness of C6 on MRI axial view.
RESULTS
The length using ultrasonography showed that the average length was 2.12 cm for the internal carotid artery, 3.04 cm for the internal jugular vein, 4.34 cm for the sternocleidomastoid muscle and 0.68 cm for the longus colli muscle. Cervical MRI was used to measure the same structures. Its results were 2.23 cm for the internal carotid artery, 3.14 cm for the internal jugular vein, 4.39 cm for the sternocleidomastoid muscle and 0.70 cm for the longus colli muscle. We also measured the thickness of the longus colli muscle with ultrasonography and cervical MRI, and the results were 0.77 cm and 0.76 cm, respectively. There was no statistically significant difference between ultrasonography and MRI for the measurement of length, but there was a statistically significant difference for the measurement of thickness.
CONCLUSION
There was a significant difference for the measurement of cervical anatomical stuctures using ultrasonography, and especially the longus coli thickness, as compared with that of MRI. Therefore, we suggest that ultrasonography can give more useful information for the diagnosis and treatment of problems in the cervical spinal field.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Comparison of Ultrasonography and Magnetic Resonance Imaging in Measurement of Lumbar Spine Anatomic Structures
Dae Moo Shim, Tae Kyun Kim, Sung Kyun Oh, Seok Jung Lee, Hee Seok Yang
J Korean Orthop Assoc. 2012;47(2):140-145. doi: 10.4055/jkoa.2012.47.2.140.Comparison of Ultrasonography and Magnetic Resonance Imaging in Measurement of Lumbar Muscles
Chang Su Kim, Young Ha Woo, Dae Moo Shim, Tae Kyun Kim, Jeong Mi Lee, Bong Jun Jang, Byung Min Yoo
J Korean Orthop Assoc. 2016;51(5):371-377. doi: 10.4055/jkoa.2016.51.5.371.
Reference
-
1. Nofsinger C, Konin JG. Diagnostic ultrasound in sports medicine: current concepts and advances. Sports Med Arthrosc. 2009. 17:25–30.2. Hodges PW, Pengel LH, Herbert RD, Gandevia SC. Measurement of muscle contraction with ultrasound imaging. Muscle Nerve. 2003. 27:682–692.
Article3. McMeeken JM, Beith ID, Newham DJ, Milligan P, Critchley DJ. The relationship between EMG and change in thickness of transversus abdominis. Clin Biomech (Bristol, Avon). 2004. 19:337–342.
Article4. Bunce SM, Moore AP, Hough AD. M-mode ultrasound: a reliable measure of transversus abdominis thickness? Clin Biomech (Bristol, Avon). 2002. 17:315–317.
Article5. Emshoff R, Bertram S, Strobl H. Ultrasonographic cross-sectional characteristics of muscles of the head and neck. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999. 87:93–106.
Article6. Kristjansson E. Reliability of ultrasonography for the cervical multifidus muscle in asymptomatic and symptomatic subjects. Man Ther. 2004. 9:83–88.
Article7. Jacobson JA. Musculoskeletal ultrasound and MRI: which do I choose? Semin Musculoskelet Radiol. 2005. 9:135–149.
Article8. Iannotti JP, Ciccone J, Buss DD, et al. Accuracy of office-based ultrasonography of the shoulder for the diagnosis of rotator cuff tears. J Bone Joint Surg Am. 2005. 87:1305–1311.
Article9. Shim DM, Kim TK, Oh SK, Choi YH, Lee SJ. Effectiveness of selective nerve root block on the need for surgical treatment of lumbar spine: a minimum 5 years follow up. J Korean Orthop Assoc. 2009. 44:118–122.10. Davies MJ, Silbert BS, Scott DA, Cook RJ, Mooney PH, Blyth C. Superficial and deep cervical plexus block for carotid artery surgery: a prospective study of 1000 blocks. Reg Anesth. 1997. 22:442–446.
Article11. Dhonneur G, Saidi NE, Merle JC, Asfazadourian H, Ndoko SK, Bloc S. Demonstration of the spread of injectate with deep cervical plexus block: a case series. Reg Anesth Pain Med. 2007. 32:116–119.
Article12. Saranteas T, Paraskeuopoulos T, Anagnostopoulou S, Kanellopoulos I, Mastoris M, Kostopanagiotou G. Ultrasound anatomy of the cervical paravertebral space: a preliminary study. Surg Radiol Anat. 2010. 32:617–622.
Article13. Suk SI. Textbook of spinal surgery. 2004. 2nd ed. Korea:14. Martinoli C, Bianchi S, Santacroce E, Pugliese F, Graif M, Derchi LE. Brachial plexus sonography: a technique for assessing the root level. AJR Am J Roentgenol. 2002. 179:699–702.
Article15. Hashimoto BE, Kramer DJ, Wiitala L. Applications of musculoskeletal sonography. J Clin Ultrasound. 1999. 27:293–318.
Article16. Iannotti JP, Ciccone J, Buss DD, et al. Accuracy of office-based ultrasonography of the shoulder for the diagnosis of rotator cuff tears. J Bone Joint Surg Am. 2005. 87:1305–1311.
Article17. Zhao J, Quan Z, Ou Y, Jiang D. Prevention and treatment of early postoperative complications of anterior cervical spinal surgery. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2008. 22:901–904.18. Lee JP, Tseng WY, Shau YW, Wang CL, Wang HK, Wang SF. Measurement of segmental cervical multifidus contraction by ultrasonography in asymptomatic adults. Man Ther. 2007. 12:286–294.
Article19. Urrutia J, Bono CM. Long-term results of surgical treatment of dysphagia secondary to cervical diffuse idiopathic skeletal hyperostosis. Spine J. 2009. 9:e13–e17.20. Miyamoto K, Sugiyama S, Hosoe H, Iinuma N, Suzuki Y, Shimizu K. Postsurgical recurrence of osteophytes causing dysphagia in patients with diffuse idiopathic skeletal hyperostosis. Eur Spine J. 2009. 18:1652–1658.
Article21. Sinnatamby CS. Sinnatamby CS, editor. Head and neck and spine. Last's anatomy. 2006. 11th ed. London: Churchill Livingstone;341–372.