J Korean Fract Soc.
2008 Apr;21(2):151-156. 10.12671/jkfs.2008.21.2.151.
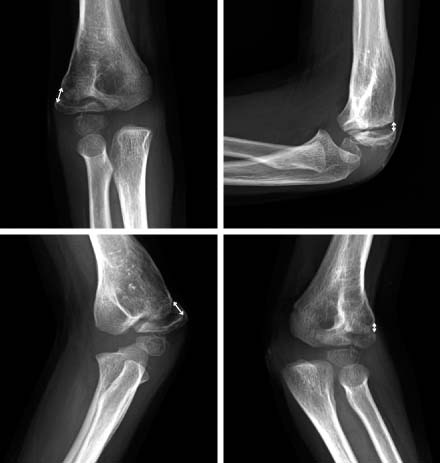
In Situ Late Metaphyseal Osteosynthesis for the Fractures of the Lateral Humeral Condyle in Children
- Affiliations
-
- 1Department of Orthopaedic Surgery, Yonsei University College of Medicine, Seoul, Korea. leeks@yuhs.ac
- KMID: 2183912
- DOI: http://doi.org/10.12671/jkfs.2008.21.2.151
Abstract
-
PURPOSE: To evaluate the efficacy of the in situ late osteosynthesis for slightly displaced fractures of the lateral humeral condyle.
MATERIALS AND METHODS
From 2000 to 2004, 12 patients (8 boys and 4 girls) were managed with in situ late osteosynthesis for fractures of the lateral humeral condyle. The average age at the time of operation was 6 years 1 month (1 year 7 months~9 years 1 month), and the mean amount of fragment displacement was 3.3 mm (2.0~4.5 mm). The operative procedure included curettage and in situ fixation of the fragment
RESULTS
Bony union was achieved in all cases after avg. 48 months (33~73 months) follow-up assessment. According to the score system of Dhillon et al, 7 patients had excellent, 3 had good, 2 had fair results. None of the patients developed avascular necrosis or premature closure of the epiphysis.
CONCLUSION
We suggest that in situ fixation is an effective method for the late treatment of slightly displaced fracture of the lateral humeral condyle.
MeSH Terms
Figure
Reference
-
1. Beaty JH, Kasser JR. Rockwood and wilkin's fractures in children. 5th ed. Philadelphia: Lippincott Williams and Wilkins;2001. p. 626–644.2. Chung MS, Lee SC. Treatment of fractures of lateral condyle of humerus with complications. J Korean Fract Soc. 1995; 8:659–666.3. De Boeck H. Surgery for nonunion of the lateral humeral condyle in children. 6 cases followed for 1-9 years. Acta Orthop Scand. 1995; 66:401–402.
Article4. Dhillon KS, Sengupta S, Singh BJ. Delayed management of fracture of the lateral humeral condyle in children. Acta Orthop Scand. 1988; 59:419–424.
Article5. Flynn JC. Nonunion of slightly displaced fractures of the lateral humeral condyle in children: an update. J Pediatr Orthop. 1989; 9:691–696.
Article6. Flynn JC, Richards JF Jr, Saltzman RI. Prevention and treatment of non-union of slightly displaced fractures of the lateral humeral condyle in children. An end-result study. J Bone Joint Surg Am. 1975; 57:1087–1092.
Article7. Foster DE, Sullivan JA, Gross RH. Lateral humeral condylar fractures in children. J Pediatr Orthop. 1985; 5:16–22.
Article8. Gaur SC, Varma AN, Swarup A. A new surgical technique for old ununited lateral condyle fractures of the humerus in children. J Trauma. 1993; 34:68–69.
Article9. Ha SH, Sohn HM, Lee JY, Oh SJ. Surgical treatment for the non-union of the lateral humeral condyle fracture using closing wedge osteotomy and bone graft. J Korean Soc Fract. 2003; 16:379–384.
Article10. Hardacre JA, Nahigian SH, Froimson AI, Brown JE. Fractures of the lateral condyle of the humerus in children. J Bone Joint Surg Am. 1971; 53:1083–1095.
Article11. Inoue G, Tamura Y. Osteosynthesis for longstanding nonunion of the lateral humeral condyle. Arch Orthop Trauma Surg. 1993; 112:236–238.
Article12. Jakob R, Fowles JV, Rang M, Kassab MT. Observations concerning fractures of the lateral humeral condyle in children. J Bone Joint Surg Br. 1975; 57:430–436.
Article13. Masada K, Kawai H, Kawabata H, Masatomi T, Tsuyuguchi Y, Yamamoto K. Osteosynthesis for old, established non-union of the lateral condyle of the humerus. J Bone Joint Surg Am. 1990; 72:32–40.
Article14. Papandrea R, Waters PM. Posttraumatic reconstruction of the elbow in the pediatric patient. Clin Orthop Relat Res. 2000; 370:115–126.
Article15. Roye DP Jr, Bini SA, Infosino A. Late surgical treatment of lateral condylar fractures in children. J Pediatr Orthop. 1991; 11:195–199.
Article16. Shimada K, Masada K, Tada K, Yamamoto T. Osteosynthesis for the treatment of non-union of the lateral humeral condyle in children. J Bone Joint Surg Am. 1997; 79:234–240.
Article17. Skaggs DL, Flynn JM. Staying out of trouble in pediatric orthopaedics. 1st ed. Philadelphia: Lippincott Williams & Wilkins;2006. p. 66–79.18. Song KS, Kang CH, Min BW, Bae KC, Cho CH. Internal oblique radiographs for diagnosis of nondisplaced or minimally displaced lateral condylar fractures of the humerus in children. J Bone Joint Surg Am. 2007; 89:58–63.
Article19. Toh S, Tsubo K, Nishikawa S, Inoue S, Nakamura R, Narita S. Osteosynthesis for nonunion of the lateral humeral condyle. Clin Orthop Relat Res. 2002; 405:230–241.
Article20. Toh S, Tsubo K, Nishikawa S, Inoue S, Nakamura R, Harata S. Long-standing nonunion of fractures of the lateral humeral condyle. J Bone Joint Surg Am. 2002; 84:593–598.
Article21. Wattenbarger JM, Gerardi J, Johnston CE. Late open reduction internal fixation of lateral condyle fractures. J Pediatr Orthop. 2002; 22:394–398.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Osteosynthesis for Nonunion of the Lateral Condyle of the Humerus
- Treatment of Fractures of Lateral Condyle of Humerus with Compliations
- Medial and Lateral Dual Plate Fixation for Osteoporotic Proximal Humerus Comminuted Fracture: 2 Case Reports
- Minimally Invasive Plate Osteosynthesis for Humeral Proximal or Distal Shaft Fractures Using a 3.5/5.0 Metaphyseal Locking Plate
- Fracture of the Capitellum of the Bumerus: Report of 4 cases