J Korean Med Assoc.
2004 Oct;47(10):966-972. 10.5124/jkma.2004.47.10.966.
Cause and Treatment of Lymphedema
- Affiliations
-
- 1Department of Surgery / Division of Vascular Surgery, Sungkyunkwan University School of Medicine, Samsung Medical Center, Korea.
- KMID: 2183534
- DOI: http://doi.org/10.5124/jkma.2004.47.10.966
Abstract
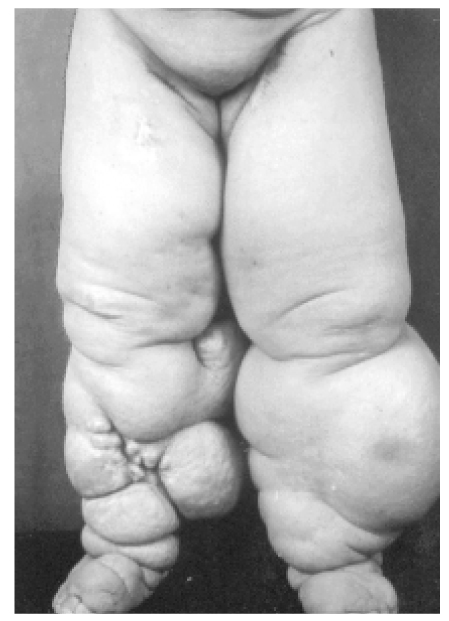
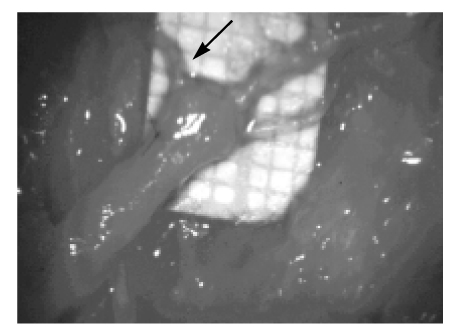
- INTRODUCTION: Lymphedema develops due to the abnormality of the transport capacity of the lymphatic system. Clinically lymphedema is not only a cosmetic deformity, but also a disabling and distressing condition. CLASSIFICATION: Primary lymphedema is an inborn defect caused by such condition as absence or underdevelopment of the lymphatic system. It occurs in approximately 1 in 10,000 persons less than 20 years of age, with females being affected more frequently than males. Secondary lymphedema is an acquired condition resulting from loss or obstruction of the previously normal lymphatic system due to infection, tumor, filariasis and other miscellaneous conditions. CLINICAL FEATURES: Clinical symptoms and signs depend on the duration and the severity of the lymphedema. In the early stage of disease, the edema is soft and pits easily with pressure (pitting edema) and may decrease or disappear with elevation of the limbs. In the advanced stage, the skin texture turns woody as the surrounding tissue becomes indurated and fibrotic. DIAGNOSIS: Lymphangiography was introduced in the early 19th century. But there are several drawbacks to this procedure, including the complexity of the procedure, irradiation by contrast agent that may result in lymphangitis and potentially worsen the lymphedema. Lymphoscintigraphy is easier to perform than lymphangiography and is not reported to cause lymphangitis. Lymphoscintigraphy is gradually replacing lymphangiography. TREATMENT: The mainstay of the treatment is complex decongestive physical therapy including leg elevation, elastic or rigid compression, manual lymph drainage, and intermittent pneumatic compression. When the function of the limb is significantly impaired, surgical reduction is considered. The surgery is not curative, but it can make the disorder more manageable by complex decongestive physical therapy.
MeSH Terms
Figure
Reference
-
2. Kim DI, Huh S, Hwang JH, Kim YI. Venous dynamics in leg lymphedema. Lymphology. 1999. 32:11–14.7. Cambria RA, Gloviczki P, Naessens JM, Wahner HW. Noninvasive evaluation of the lymphatic systems with lymphoscintigraphy : A prospective semiquantitative analysis in 386 extremities. J Vasc Surg. 1993. 18:773–782.
Article8. Hwang JH, Kwon JY, Lee KW, Choi JY, Kim BT, Kim DI, et al. Changes in lymphatic function after complex physical therapy for lymphedema. Lymphology. 1999. 32:15–21.9. Casley-Smith JR. Modern treatment of lymphoedema. I. Complex physical therapy: The first 200 Australian limbs. Australas J Dermatol. 1992. 33:61–68.
Article10. Dini D, DelMastro L, Gozza A. The role of pnematic compression in the treatment of postmastectomy lymphedema: A randomized phase III study. Ann Oncol. 1998. 9:187–190.
Article12. Casley-Smith JR, Morgan RG, Piuller NB. Treatment of lymphedema of the arms and legs with 5,6-benzo-a-pyrone. N Engl J Med. 1993. 329:1158–1163.
Article13. Kim DI, Huh SH, Hwang JH, Joh JH. Excisional surgery for chronic advanced lymphedema. Surgery Today. 2004. 34:134–137.
Article14. Kim DI, Huh S, Lee SJ, Hwang JH, Kim YI. Excision of subcutaneou tissue and deep muscle fascia for advanced lymphedema. Lymphology. 1998. 31:190–194.15. Dumanian GA, Futrell JW. Radical excision and delayed reconstruction of a lymphedematous leg with a 15 year follow-up. Lymphology. 1996. 29:20–24.16. Mavilli ME, Naldoken S, Safak Y. Modified Charles operation for primary fibrosclerotic lymphedema. Lymphology. 1994. 27:14–20.17. O'Brien BM, Mellow CG, Khazanchi RK. Long term results after micro-lyphatico-venous anastomoses for the treatment of obstructive lymphedema. Plast Reconstr Surg. 1990. 85:562–572.