J Adv Prosthodont.
2013 Nov;5(4):428-433. 10.4047/jap.2013.5.4.428.
In vitro evaluation of resonance frequency analysis values to different implant contact ratio and stiffness of surrounding material
- Affiliations
-
- 1Department of Prosthodontics, Graduate School of Clinical Dental Science, The Catholic University of Korea, Seoul, Republic of Korea.
- 2Department of Prosthodontics, Samsung Medical Center, College of Medicine, Sungkyunkwan University, Seoul, Republic of Korea. seokgyu_k@hanmail.net
- KMID: 2176534
- DOI: http://doi.org/10.4047/jap.2013.5.4.428
Abstract
- PURPOSE
The present study was aimed to evaluate the influence of implant contact ratio and stiffness of implant-surrounding materials on the resonance frequency analysis (RFA) values.
MATERIALS AND METHODS
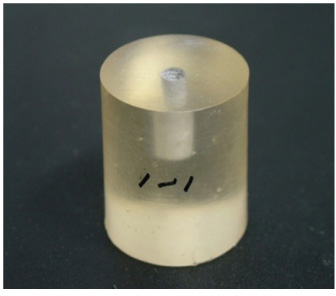
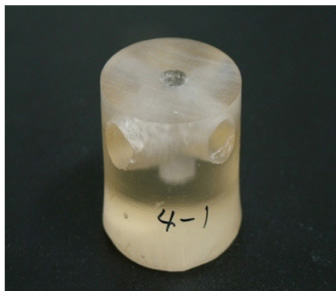
Seventy resin blocks that had the different amounts (100, 50, 30, 15%) of resin-implant contact (RIC) were fabricated. Ten silicone putty blocks with 100% silicone-implant contact were also made. The implants with O5.0 mm x 13.0 mm were placed on eighty specimen blocks. The RFA value was measured on the transducer that was connected to each implant by Osstell Mentor. Kruskal-Wallis and Scheffe's tests (alpha=.05) were done for statistical analysis.
RESULTS
The control resin group with 100% RIC had the highest RFA value of 83.9, which was significantly different only from the resin group with 15% RIC among the resin groups. The silicone putty group with 100% contact had the lowest RFA value of 36.6 and showed statistically significant differences from the resin groups.
CONCLUSION
Within the limitations of this in vitro study, there was no significant difference in the RFA values among the resin groups with different RIC's except when the RIC difference was more than 85%. A significant increase in the RFA value was observed related to the increase in stiffness of material around implant.
Keyword
MeSH Terms
Figure
Reference
-
1. Schulte W, Lukas D. Periotest to monitor osseointegration and to check the occlusion in oral implantology. J Oral Implantol. 1993; 19:23–32.2. Meredith N, Alleyne D, Cawley P. The application of modal vibration analysis to study bone healing in vivo. J Dent Res. 1994; 73:793.3. Becker W, Sennerby L, Bedrossian E, Becker BE, Lucchini JP. Implant stability measurements for implants placed at the time of extraction: a cohort, prospective clinical trial. J Periodontol. 2005; 76:391–397.4. Zix J, Kessler-Liechti G, Mericske-Stern R. Stability measurements of 1-stage implants in the maxilla by means of resonance frequency analysis: a pilot study. Int J Oral Maxillofac Implants. 2005; 20:747–752.5. Meredith N, Shagaldi F, Alleyne D, Sennerby L, Cawley P. The application of resonance frequency measurements to study the stability of titanium implants during healing in the rabbit tibia. Clin Oral Implants Res. 1997; 8:234–243.6. Schliephake H, Sewing A, Aref A. Resonance frequency measurements of implant stability in the dog mandible: experimental comparison with histomorphometric data. Int J Oral Maxillofac Surg. 2006; 35:941–946.7. Scarano A, Degidi M, Iezzi G, Petrone G, Piattelli A. Correlation between implant stability quotient and bone-implant contact: a retrospective histological and histomorphometrical study of seven titanium implants retrieved from humans. Clin Implant Dent Relat Res. 2006; 8:218–222.8. Turkyilmaz I, Sennerby L, McGlumphy EA, Tözüm TF. Biomechanical aspects of primary implant stability: a human cadaver study. Clin Implant Dent Relat Res. 2009; 11:113–119.9. Sim CP, Lang NP. Factors influencing resonance frequency analysis assessed by Osstell mentor during implant tissue integration: I. Instrument positioning, bone structure, implant length. Clin Oral Implants Res. 2010; 21:598–604.10. Nkenke E, Hahn M, Weinzierl K, Radespiel-Tröger M, Neukam FW, Engelke K. Implant stability and histomorphometry: a correlation study in human cadavers using stepped cylinder implants. Clin Oral Implants Res. 2003; 14:601–609.11. Miyamoto I, Tsuboi Y, Wada E, Suwa H, Iizuka T. Influence of cortical bone thickness and implant length on implant stability at the time of surgery-clinical, prospective, biomechanical, and imaging study. Bone. 2005; 37:776–780.12. Ostman PO, Hellman M, Wendelhag I, Sennerby L. Resonance frequency analysis measurements of implants at placement surgery. Int J Prosthodont. 2006; 19:77–83.13. Trisi P, Carlesi T, Colagiovanni M, Perfetti G. Implant stability quotient (ISQ) vs direct in vitro measurement of primary stability(micromotion): effect of bone density and insertion torque. J Osteol Biomat. 2010; 1:141–151.14. da Cunha HA, Francischone CE, Filho HN, de Oliveira RC. A comparison between cutting torque and resonance frequency in the assessment of primary stability and final torque capacity of standard and TiUnite single-tooth implants under immediate loading. Int J Oral Maxillofac Implants. 2004; 19:578–585.15. O'Brien WJ. Dental materials and their selection. 3rd ed. Chicago: Quintessence;2002. p. 328–330.16. Albrektsson T, Brånemark PI, Hansson HA, Lindström J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981; 52:155–170.17. Albrektsson T. Dental implants: a review of clinical approaches. Aust Prosthodont Soc Bull. 1985; 15:7–25.18. Albrektsson T, Jacobsson M. Bone-metal interface in osseointegration. J Prosthet Dent. 1987; 57:597–607.19. Zarb GA, Albrektsson T. Osseointegration: a requiem for the periodontal ligament? Int J Periodont Res Dent. 1991; 11:88–91.20. Pierrisnard L, Renouard F, Renault P, Barquins M. Influence of implant length and bicortical anchorage on implant stress distribution. Clin Implant Dent Relat Res. 2003; 5:254–262.21. Hansson S. A conical implant-abutment interface at the level of the marginal bone improves the distribution of stresses in the supporting bone. An axisymmetric finite element analysis. Clin Oral Implants Res. 2003; 14:286–293.22. Bozkaya D, Muftu S, Muftu A. Evaluation of load transfer characteristics of five different implants in compact bone at different load levels by finite elements analysis. J Prosthet Dent. 2004; 92:523–530.23. Cehreli MC, Akça K, Iplikçioğlu H. Force transmission of one- and two-piece morse-taper oral implants: a nonlinear finite element analysis. Clin Oral Implants Res. 2004; 15:481–489.24. Kitamura E, Stegaroiu R, Nomura S, Miyakawa O. Biomechanical aspects of marginal bone resorption around osseointegrated implants: considerations based on a three-dimensional finite element analysis. Clin Oral Implants Res. 2004; 15:401–412.25. Martinez H, Davarpanah M, Missika P, Celletti R, Lazzara R. Optimal implant stabilization in low density bone. Clin Oral Implants Res. 2001; 12:423–432.26. Meredith N, Alleyne D, Cawley P. Quantitative determination of the stability of the implant-tissue interface using resonance frequency analysis. Clin Oral Implants Res. 1996; 7:261–267.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The relationship between initial implant stability quotient values and bone-to-implant contact ratio in the rabbit tibia
- Effect of bone quality and implant surgical technique on implant stability quotient (ISQ) value
- Correlation assessment between resonance frequency analysis and radiographic method according to peri-implant bone change
- An evaluation of the primary implant stability and the immediate load-bearing capacity according to the change of cortical bone thickness
- Bone response of three different surface implants : Histomorphometric, perio test value and resonance frequency analysis in beagle dogs