Intest Res.
2015 Jul;13(3):266-273. 10.5217/ir.2015.13.3.266.
Efficacy of Thiopurines in Biologic-Naive Japanese Patients With Crohn's Disease: A Single-Center Experience
- Affiliations
-
- 1Department of Gastroenterology & Hepatology, Graduate School of Medicine, Kyoto University, Kyoto, Japan. hiropy_n@kuhp.kyoto-u.ac.jp
- 2The Third Department of Internal Medicine, Kansai Medical University, Osaka, Japan.
- 3Department of Internal Medicine, Faculty of Medicine, Al-Azhar University, Cairo, Egypt.
- KMID: 2174482
- DOI: http://doi.org/10.5217/ir.2015.13.3.266
Abstract
- BACKGROUND/AIMS
Early use of biologics in patients with Crohn's disease (CD) improves quality of life. However, the effects of the early use of immunomodulators on long-term outcomes remain unclear. This study aimed to evaluate the effects of immunomodulators in patients with CD.
METHODS
Between January 2004 and December 2011, 47 biologic-naive CD patients treated with thiopurines alone for remission maintenance were analyzed. The patients were classified into 2 groups depending on the presence or absence of digestive complications. We evaluated the efficacy of and predictive factors for thiopurine use for remission maintenance.
RESULTS
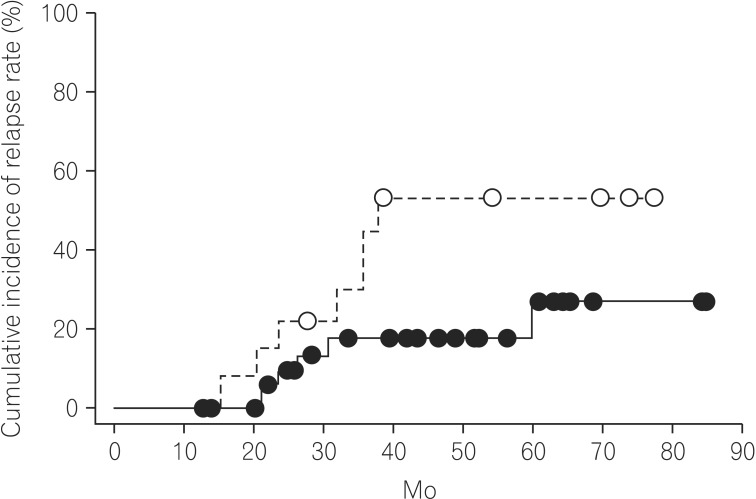
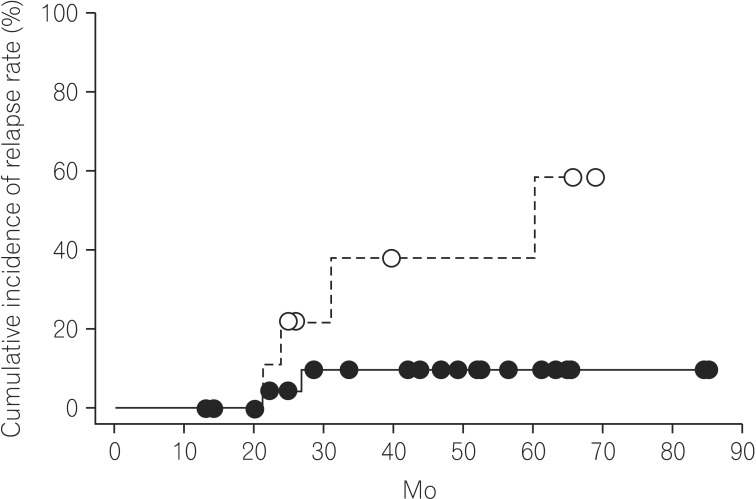
The cumulative relapse rates at 24 and 60 months were 13.7% and 35.4%, respectively. Regarding patient characteristics, there was a significant difference in patient history of surgery between the non-relapse and relapse groups (P=0.021). The cumulative relapse rate was lower in patients without a history of surgery than in those with such a history (27.2% and 52.9% at 60.0 months, respectively). Multivariate analysis suggested that the prevalence of stricturing and penetrating complications is an independent factor for relapse. The cumulative relapse rate in patients without a history of surgery was significantly lower in the non-stricturing and non-penetrating group than in the stricturing and penetrating group (11.8% at 85.0 months vs. 58.5% at 69.0 months; P=0.036).
CONCLUSIONS
Thiopurine use might be beneficial for the long-term maintenance of remission in biologic-naive Crohn's disease patients without digestive complications and a history of surgery.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
NUDT15 ,FTO , andRUNX1 genetic variants and thiopurine intolerance among Japanese patients with inflammatory bowel diseases
Toshiyuki Sato, Tetsuya Takagawa, Yoichi Kakuta, Akihiro Nishio, Mikio Kawai, Koji Kamikozuru, Yoko Yokoyama, Yuko Kita, Takako Miyazaki, Masaki Iimuro, Nobuyuki Hida, Kazutoshi Hori, Hiroki Ikeuchi, Shiro Nakamura
Intest Res. 2017;15(3):328-337. doi: 10.5217/ir.2017.15.3.328.
Reference
-
1. Pariente B, Cosnes J, Danese S, et al. Development of the Crohn's disease digestive damage score, the Lémann score. Inflamm Bowel Dis. 2011; 17:1415–1422. PMID: 21560202.
Article2. Anthonisen P, Barany F, Folkenborg O, et al. The clinical effect of salazosulphapyridine (Salazopyrin r) in Crohn's disease. A controlled double-blind study. Scand J Gastroenterol. 1974; 9:549–554. PMID: 4153646.
Article3. Travis SP, Stange EF, Lémann M, et al. European evidence based consensus on the diagnosis and management of Crohn's disease: current management. Gut. 2006; 55(Suppl 1):i16–i35. PMID: 16481629.
Article4. Lichtenstein GR, Hanauer SB, Sandborn WJ. Practice Parameters Committee of American College of Gastroenterology. Management of Crohn's disease in adults. Am J Gastroenterol. 2009; 104:465–483. PMID: 19174807.
Article5. Colombel JF, Sandborn WJ, Reinisch W, et al. Infliximab, azathioprine, or combination therapy for Crohn's disease. N Engl J Med. 2010; 362:1383–1395. PMID: 20393175.
Article6. Colombel JF, Sandborn WJ, Rutgeerts P, et al. Adalimumab for maintenance of clinical response and remission in patients with Crohn's disease: the CHARM trial. Gastroenterology. 2007; 132:52–65. PMID: 17241859.
Article7. Peyrin-Biroulet L, Oussalah A, Williet N, Pillot C, Bresler L, Bigard MA. Impact of azathioprine and tumour necrosis factor antagonists on the need for surgery in newly diagnosed Crohn's disease. Gut. 2011; 60:930–936. PMID: 21228429.
Article8. Keane J, Gershon S, Wise RP, et al. Tuberculosis associated with infliximab, a tumor necrosis factor a-neutralizing agent. N Engl J Med. 2001; 345:1098–1104. PMID: 11596589.
Article9. Mackey AC, Green L, Liang LC, Dinndorf P, Avigan M. Hepatosplenic T cell lymphoma associated with infliximab use in young patients treated for inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2007; 44:265–267. PMID: 17255842.
Article10. Panés J, López-Sanromán A, Bermejo F, et al. Early azathioprine therapy is no more effective than placebo for newly diagnosed Crohn's disease. Gastroenterology. 2013; 145:766–774. PMID: 23770132.
Article11. Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006; 55:749–753. PMID: 16698746.
Article12. Sandborn WJ. Rational dosing of azathioprine and 6-mercaptopurine. Gut. 2001; 48:591–592. PMID: 11302950.
Article13. Best WR, Becktel JM, Singleton JW, Kern F Jr. Development of a Crohn's disease activity index. National Cooperative Crohn's Disease Study. Gastroenterology. 1976; 70:439–444. PMID: 1248701.14. Van Assche G, Dignass A, Reinisch W, et al. The second European evidence-based Consensus on the diagnosis and management of Crohn's disease: Special situations. J Crohns Colitis. 2010; 4:63–101. PMID: 21122490.15. Daperno M, D'Haens G, Van Assche G, et al. Development and validation of a new, simplified endoscopic activity score for Crohn's disease: the SES-CD. Gastrointest Endosc. 2004; 60:505–512. PMID: 15472670.
Article16. Stange EF, Travis SP, Vermeire S, et al. European evidence-based Consensus on the diagnosis and management of ulcerative colitis: Definitions and diagnosis. J Crohns Colitis. 2008; 2:1–23. PMID: 21172194.
Article17. Prefontaine E, Sutherland LR, Macdonald JK, Cepoiu M. Azathioprine or 6-mercaptopurine for maintenance of remission in Crohn's disease. Cochrane Database Syst Rev. 10.1002/14651858.CD000067.pub2. Published online 21 January 2009.
Article18. Markowitz J, Grancher K, Kohn N, Lesser M, Daum F. A multicenter trial of 6-mercaptopurine and prednisone in children with newly diagnosed Crohn's disease. Gastroenterology. 2000; 119:895–902. PMID: 11040176.
Article19. Lakatos PL, Golovics PA, Dávid G, et al. Has there been a change in the natural history of Crohn's disease? Surgical rates and medical management in a population-based inception cohort from Western Hungary between 1977-2009. Am J Gastroenterol. 2012; 107:579–588. PMID: 22233693.
Article20. Bouhnik Y, Lémann M, Mary JY, et al. Long-term follow-up of patients with Crohn's disease treated with azathioprine or 6-mercaptopurine. Lancet. 1996; 347:215–219. PMID: 8551879.
Article21. Jaspers GJ, Verkade HJ, Escher JC, de Ridder L, Taminiau JA, Rings EH. Azathioprine maintains first remission in newly diagnosed pediatric Crohn's disease. Inflamm Bowel Dis. 2006; 12:831–836. PMID: 16954801.
Article22. Candy S, Wright J, Gerber M, Adams G, Gerig M, Goodman R. A controlled double blind study of azathioprine in the management of Crohn's disease. Gut. 1995; 37:674–678. PMID: 8549944.
Article23. Kwak MS, Kim DH, Park SJ, et al. Efficacy of early immunomodulator therapy on the outcomes of Crohn's disease. BMC Gastroenterol. 2014; 14:85. PMID: 24886458.
Article24. Cosnes J, Bourrier A, Laharie D, et al. Early administration of azathioprine vs conventional management of Crohn's Disease: a randomized controlled trial. Gastroenterology. 2013; 145:758–765. PMID: 23644079.
Article25. D'Haens G, Baert F, van Assche G, et al. Early combined immunosuppression or conventional management in patients with newly diagnosed Crohn's disease: an open randomised trial. Lancet. 2008; 371:660–667. PMID: 18295023.26. Peyrin-Biroulet L, Deltenre P, Ardizzone S, et al. Azathioprine and 6-mercaptopurine for the prevention of postoperative recurrence in Crohn's disease: a meta-analysis. Am J Gastroenterol. 2009; 104:2089–2096. PMID: 19568226.
Article27. Golovics PA, Lakatos PL, Dávid G, et al. The effect of early immunosuppressive therapy on the rate of resections performed in patients with Chron's disease, in Veszprém county, Hungary, a population-based cohort study. Orv Hetil. 2012; 153:541–552. PMID: 22450143.
Article28. Lennard-Jones JE, Stalder GA. Prognosis after resection of chronic regional ileitis. Gut. 1967; 8:332–336. PMID: 6039720.
Article29. Hellers G. Crohn's disease in Stockholm county 1955-1974. A study of epidemiology, results of surgical treatment and long-term prognosis. Acta Chir Scand Suppl. 1979; 490:1–84. PMID: 293116.30. López-Martín C, Chaparro M, Espinosa L, Bejerano A, Maté J, Gisbert JP. Adverse events of thiopurine immunomodulators in patients with inflammatory bowel disease. Gastroenterol Hepatol. 2011; 34:385–392. PMID: 21616565.
Article31. Lichtenstein GR, Abreu MT, Cohen R, Tremaine W. American Gastroenterological Association. American Gastroenterological Association Institute medical position statement on corticosteroids, immunomodulators, and infliximab in inflammatory bowel disease. Gastroenterology. 2006; 130:935–939. PMID: 16530531.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Biologic therapies in Crohn's disease
- Treatment of inflammatory bowel diseases: focusing on biologic agents and new therapies
- Early Biologic Treatment in Pediatric Crohn's Disease: Catching the Therapeutic Window of Opportunity in Early Disease by Treat-to-Target
- Efficacy of biologic therapies for biologic-naïve Japanese patients with moderately to severely active ulcerative colitis: a network meta-analysis
- Natural Course of Crohn's Disease and Novel Treatment Drugs