Intest Res.
2014 Jul;12(3):221-228. 10.5217/ir.2014.12.3.221.
Is Colonoscopy Necessary after Computed Tomography Diagnosis of Acute Diverticulitis?
- Affiliations
-
- 1Department of Gastroenterology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. younghokim@skku.edu
- 2Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2174381
- DOI: http://doi.org/10.5217/ir.2014.12.3.221
Abstract
- BACKGROUND/AIMS
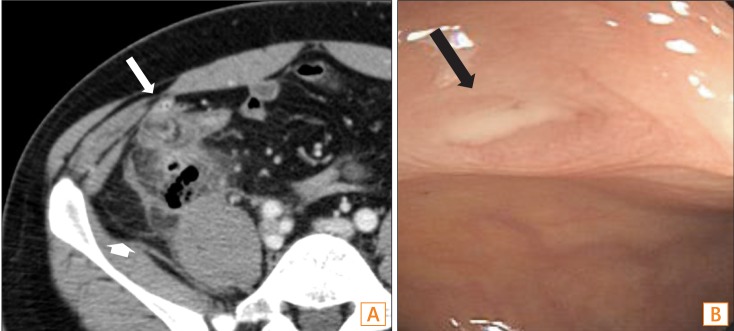
A diagnosis of acute diverticulitis is based on computed tomography (CT). Colonoscopy is commonly performed after the acute event to exclude other diagnoses. This study aimed to determine whether colonoscopy is necessary and what additional information is gained from a colonoscopy after acute diverticulitis.
METHODS
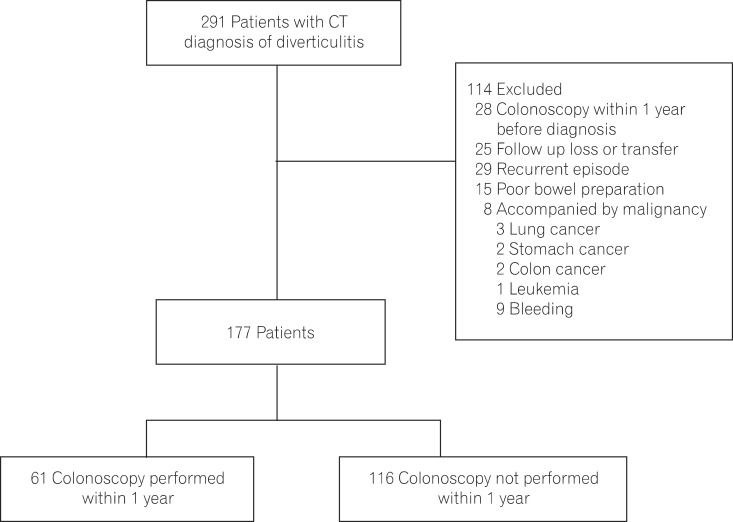
Acute diverticulitis was diagnosed by clinical criteria and characteristic CT findings. We analyzed the number of patients in whom colorectal cancers were diagnosed and other incidental findings of polyps and other diseases.
RESULTS
A total of 177 patients were analyzed retrospectively. The mean age was 43.3+/-15.3 years (range, 13-82 years) and 97 patients (54.8%) were male. Sixty-one patients had undergone a colonoscopy within 1 year of the acute attack. Advanced adenomatous lesions and colonic malignancy were not detected. Nineteen patients (31.1%) had > or =1 polyp and 11 patients (18.0%) had an adenomatous polyp. No new or different diagnosis was made after colonoscopy. None of the 116 patients who did not undergo colonoscopy within a year after acute diverticulitis had a diagnosis of colorectal cancer registered with the Korea Central Cancer Registry.
CONCLUSIONS
Routine colonoscopy yields little benefit in patients with acute diverticulitis diagnosed by typical clinical symptoms and CT. The current practice of a colonoscopy after acute diverticulitis needs to be reevaluated.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Diagnosis and Treatment of Colonic Diverticular Disease
You Sun Kim
Korean J Gastroenterol. 2022;79(6):233-243. doi: 10.4166/kjg.2022.072.Comparative outcomes of acute colonic diverticulitis in immunocompromised versus immunocompetent patients: a systematic review and meta-analysis
Jae Gon Lee, Yong Eun Park, Ji Young Chang, Hyun Joo Song, Duk Hwan Kim, Young Joo Yang, Byung Chang Kim, Shin Hee Lee, Myung-Won You, Seong-Eun Kim
Intest Res. 2023;21(4):481-492. doi: 10.5217/ir.2023.00005.
Reference
-
1. Cho KC, Morehouse HT, Alterman DD, Thornhill BA. Sigmoid diverticulitis: diagnostic role of CT--comparison with barium enema studies. Radiology. 1990; 176:111–115. PMID: 2191360.
Article2. Rao PM. CT of diverticulitis and alternative conditions. Semin Ultrasound CT MR. 1999; 20:86–93. PMID: 10222517.
Article3. Ambrosetti P, Jenny A, Becker C, Terrier TF, Morel P. Acute left colonic diverticulitis--compared performance of computed tomography and water-soluble contrast enema: prospective evaluation of 420 patients. Dis Colon Rectum. 2000; 43:1363–1367. PMID: 11052512.
Article4. Lameris W, van Randen A, Bipat S, Bossuyt PM, Boermeester MA, Stoker J. Graded compression ultrasonography and computed tomography in acute colonic diverticulitis: meta-analysis of test accuracy. Eur Radiol. 2008; 18:2498–2511. PMID: 18523784.
Article5. Pradel JA, Adell JF, Taourel P, Djafari M, Monnin-Delhom E, Bruel JM. Acute colonic diverticulitis: prospective comparative evaluation with US and CT. Radiology. 1997; 205:503–512. PMID: 9356636.
Article6. Rao PM, Rhea JT, Novelline RA, et al. Helical CT with only colonic contrast material for diagnosing diverticulitis: prospective evaluation of 150 patients. AJR Am J Roentgenol. 1998; 170:1445–1449. PMID: 9609151.7. Ben Yaacoub I, Boulay-Coletta I, Julles MC, Zins M. CT findings of misleading features of colonic diverticulitis. Insights Imaging. 2011; 2:69–84. PMID: 22347935.8. Rafferty J, Shellito P, Hyman NH, Buie WD. Practice parameters for sigmoid diverticulitis. Dis Colon Rectum. 2006; 49:939–944. PMID: 16741596.9. Jacobs DO. Clinical practice. Diverticulitis. N Engl J Med. 2007; 357:2057–2066. PMID: 18003962.10. Choi CS, Choi SC, Seo GS, et al. Association between diverticulosis and colonic neoplasm in Koreans. Korean J Gastroenterol. 2007; 49:364–368. PMID: 17641554.11. Kieff BJ, Eckert GJ, Imperiale TF. Is diverticulosis associated with colorectal neoplasia? A cross-sectional colonoscopic study. Am J Gastroenterol. 2004; 99:2007–2011. PMID: 15447764.
Article12. Stefansson T, Ekbom A, Sparen P, Pahlman L. Increased risk of left sided colon cancer in patients with diverticular disease. Gut. 1993; 34:499–502. PMID: 8491397.
Article13. Morini S, Hassan C, Zullo A, et al. Diverticular disease as a risk factor for sigmoid colon adenomas. Dig Liver Dis. 2002; 34:635–639. PMID: 12405250.
Article14. Krones CJ, Klinge U, Butz N, et al. The rare epidemiologic coincidence of diverticular disease and advanced colonic neoplasia. Int J Colorectal Dis. 2006; 21:18–24. PMID: 15889263.
Article15. Lam TJ, Meurs-Szojda MM, Gundlach L, et al. There is no increased risk for colorectal cancer and adenomas in patients with diverticulitis: a retrospective longitudinal study. Colorectal Dis. 2010; 12:1122–1126. PMID: 19575738.
Article16. Meurs-Szojda MM, Terhaar sive Droste JS, Kuik DJ, Mulder CJ, Felt-Bersma RJ. Diverticulosis and diverticulitis form no risk for polyps and colorectal neoplasia in 4,241 colonoscopies. Int J Colorectal Dis. 2008; 23:979–984. PMID: 18594842.
Article17. Sakhnini E, Lahat A, Melzer E, et al. Early colonoscopy in patients with acute diverticulitis: results of a prospective pilot study. Endoscopy. 2004; 36:504–507. PMID: 15202046.
Article18. Lau KC, Spilsbury K, Farooque Y, et al. Is colonoscopy still mandatory after a CT diagnosis of left-sided diverticulitis: can colorectal cancer be confidently excluded? Dis Colon Rectum. 2011; 54:1265–1270. PMID: 21904141.
Article19. Lahat A, Yanai H, Menachem Y, Avidan B, Bar-Meir S. The feasibility and risk of early colonoscopy in acute diverticulitis: a prospective controlled study. Endoscopy. 2007; 39:521–524. PMID: 17554647.
Article20. Lee SJ, Kim SA, Ku BH, et al. Association between colorectal cancer and colonic diverticulosis: case-control study based on computed tomographic colonography. Abdom Imaging. 2012; 37:70–73. PMID: 21516446.
Article21. Hemming J, Floch M. Features and management of colonic diverticular disease. Curr Gastroenterol Rep. 2010; 12:399–407. PMID: 20694839.
Article22. Destigter KK, Keating DP. Imaging update: acute colonic diverticulitis. Clin Colon Rectal Surg. 2009; 22:147–155. PMID: 20676257.
Article23. Smoot RL, Gostout CJ, Rajan E, et al. Is early colonoscopy after admission for acute diverticular bleeding needed? Am J Gastroenterol. 2003; 98:1996–1999. PMID: 14499777.
Article24. Foutch PG, Zimmerman K. Diverticular bleeding and the pigmented protuberance (sentinel clot): clinical implications, histopathological correlation, and results of endoscopic intervention. Am J Gastroenterol. 1996; 91:2589–2593. PMID: 8946992.25. Savides TJ, Jensen DM. Colonoscopic hemostasis for recurrent diverticular hemorrhage associated with a visible vessel: a report of three cases. Gastrointest Endosc. 1994; 40:70–73. PMID: 8163141.
Article26. Aronchick CA, Lipshutz WH, Wright SH, Dufrayne F, Bergman G. A novel tableted purgative for colonoscopic preparation: efficacy and safety comparisons with Colyte and Fleet Phospho-Soda. Gastrointest Endosc. 2000; 52:346–352. PMID: 10968848.
Article27. Bauer VP. Emergency management of diverticulitis. Clin Colon Rectal Surg. 2009; 22:161–168. PMID: 20676259.
Article28. Wolff JH, Rubin A, Potter JD, et al. Clinical significance of colonoscopic findings associated with colonic thickening on computed tomography: is colonoscopy warranted when thickening is detected? J Clin Gastroenterol. 2008; 42:472–475. PMID: 18344892.
Article29. Cai Q, Baumgarten DA, Affronti JP, Waring JP. Incidental findings of thickening luminal gastrointestinal organs on computed tomography: an absolute indication for endoscopy. Am J Gastroenterol. 2003; 98:1734–1737. PMID: 12907326.
Article30. Shen SH, Chen JD, Tiu CM, et al. Differentiating colonic diverticulitis from colon cancer: the value of computed tomography in the emergency setting. J Chin Med Assoc. 2005; 68:411–418. PMID: 16187597.
Article31. Jang HJ, Lim HK, Lee SJ, Lee WJ, Kim EY, Kim SH. Acute diverticulitis of the cecum and ascending colon: the value of thin-section helical CT findings in excluding colonic carcinoma. AJR Am J Roentgenol. 2000; 174:1397–1402. PMID: 10789802.32. Chintapalli KN, Chopra S, Ghiatas AA, Esola CC, Fields SF, Dodd GD 3rd. Diverticulitis versus colon cancer: differentiation with helical CT findings. Radiology. 1999; 210:429–435. PMID: 10207426.
Article33. Levin TR, Zhao W, Conell C, et al. Complications of colonoscopy in an integrated health care delivery system. Ann Intern Med. 2006; 145:880–886. PMID: 17179057.
Article34. Westwood DA, Eglinton TW, Frizelle FA. Routine colonoscopy following acute uncomplicated diverticulitis. Br J Surg. 2011; 98:1630–1634. PMID: 21713756.
Article35. Sai VF, Velayos F, Neuhaus J, Westphalen AC. Colonoscopy after CT diagnosis of diverticulitis to exclude colon cancer: a systematic literature review. Radiology. 2012; 263:383–390. PMID: 22517956.
Article36. Schmilovitz-Weiss H, Yalunin E, Boaz M, et al. Does a colonoscopy after acute diverticulitis affect its management?: a single center experience. J Clin Gastroenterol. 2012; 46:317–320. PMID: 22186742.37. Boulos PB, Karamanolis DG, Salmon PR, Clark CG. Is colonoscopy necessary in diverticular disease? Lancet. 1984; 1:95–96. PMID: 6140435.
Article38. Takano M, Yamada K, Sato K. An analysis of the development of colonic diverticulosis in the Japanese. Dis Colon Rectum. 2005; 48:2111–2116. PMID: 16228844.
Article39. Simpson J, Neal KR, Scholefield JH, Spiller RC. Patterns of pain in diverticular disease and the influence of acute diverticulitis. Eur J Gastroenterol Hepatol. 2003; 15:1005–1010. PMID: 12923374.
Article40. Kim HU, Kim YH, Choe WH, et al. Clinical characteristics of colonic diverticulitis in Koreans. Korean J Gastroenterol. 2003; 42:363–368. PMID: 14646572.41. Lee SJ, Shin JE, Cho SY, et al. Clinical predictors associated with the severity of colonic diverticulitis. Intest Res. 2013; 11:23–27.
Article42. Erlinger TP, Platz EA, Rifai N, Helzlsouer KJ. C-reactive protein and the risk of incident colorectal cancer. JAMA. 2004; 291:585–590. PMID: 14762037.
Article43. Bauer KM, Hummon AB, Buechler S. Right-side and left-side colon cancer follow different pathways to relapse. Mol Carcinog. 2012; 51:411–421. PMID: 21656576.
Article