J Gynecol Oncol.
2011 Dec;22(4):260-268. 10.3802/jgo.2011.22.4.260.
Thoracic metastasis in advanced ovarian cancer: comparison between computed tomography and video-assisted thoracic surgery
- Affiliations
-
- 1Department of Radiology, Memorial Sloan-Kettering Cancer Center, New York, USA. hricakh@mskcc.org
- 2Department of Radiology, Addenbrooke's Hospital, University of Cambridge, Cambridge, UK.
- 3Department of Surgery, Memorial Sloan-Kettering Cancer Center, New York, USA.
- KMID: 2173628
- DOI: http://doi.org/10.3802/jgo.2011.22.4.260
Abstract
OBJECTIVE
To determine which computed tomography (CT) imaging features predict pleural malignancy in patients with advanced epithelial ovarian carcinoma (EOC) using video-assisted thoracic surgery (VATS), pathology, and cytology findings as the reference standard.
METHODS
This retrospective study included 44 patients with International Federation of Obstetrics and Gynecology (FIGO) stage III or IV primary or recurrent EOC who had chest CT < or =30 days before VATS. Two radiologists independently reviewed the CT studies and recorded the presence and size of pleural effusions and of ascites; pleural nodules, thickening, enhancement, subdiaphragmatic tumour deposits and supradiaphragmatic, mediastinal, hilar, and retroperitoneal adenopathy; and peritoneal seeding. VATS, pathology, and cytology findings constituted the reference standard.
RESULTS
In 26/44 (59%) patients, pleural biopsies were malignant. Only the size of left-sided pleural effusion (reader 1: rho=-0.39, p=0.01; reader 2: rho=-0.37, p=0.01) and presence of ascites (reader 1: rho=-0.33, p=0.03; reader 2: rho=-0.35, p=0.03) were significantly associated with solid pleural metastasis. Pleural fluid cytology was malignant in 26/35 (74%) patients. Only the presence (p=0.03 for both readers) and size (reader 1: rho=0.34, p=0.04; reader 2: rho=0.33, p=0.06) of right-sided pleural effusion were associated with malignant pleural effusion. Interobserver agreement was substantial (kappa=0.78) for effusion size and moderate (kappa=0.46) for presence of solid pleural disease. No other CT features were associated with malignancy at biopsy or cytology.
CONCLUSION
In patients with advanced EOC, ascites and left-sided pleural effusion size were associated with solid pleural metastasis, while the presence and size of right-sided effusion were associated with malignant pleural effusion. No other CT features evaluated were associated with pleural malignancy.
Keyword
MeSH Terms
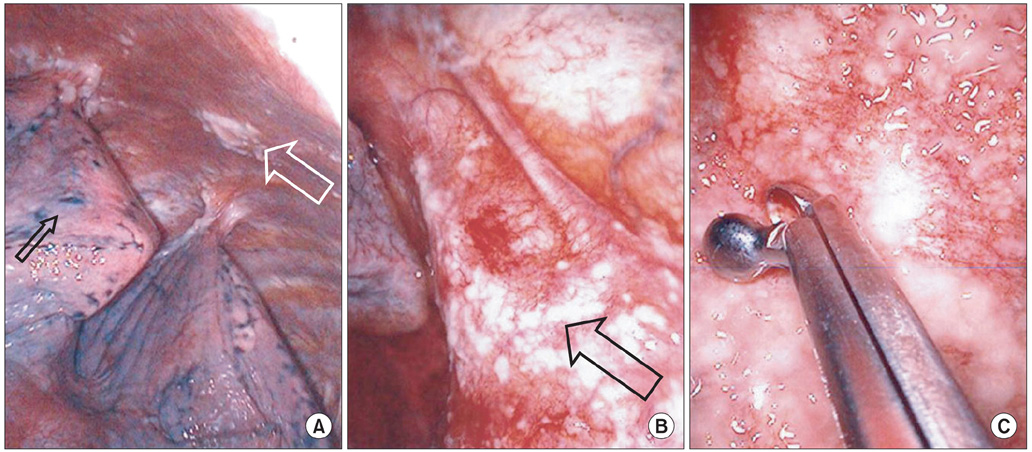
Figure
Reference
-
1. Sankaranarayanan R, Ferlay J. Worldwide burden of gynaecological cancer: the size of the problem. Best Pract Res Clin Obstet Gynaecol. 2006. 20:207–225.2. FIGO Committee on Gynecologic Oncology. Denny L, Hacker NF, Gori J, Johns HW III, Ngan HY, et al. Staging classifications and clinical practice guidelines for gynecologic cancers. 2000. Oxford: Elsevier.3. Ozols RF. Update on Gynecologic Oncology Group (GOG) trials in ovarian cancer. Cancer Invest. 2004. 22:Suppl 2. 11–20.4. Chi DS, McCaughty K, Diaz JP, Huh J, Schwabenbauer S, Hummer AJ, et al. Guidelines and selection criteria for secondary cytoreductive surgery in patients with recurrent, platinum-sensitive epithelial ovarian carcinoma. Cancer. 2006. 106:1933–1939.5. Morgan RJ Jr, Alvarez RD, Armstrong DK, Boston B, Burger RA, Chen LM, et al. NCCN Clinical Practice Guidelines in Oncology: epithelial ovarian cancer. J Natl Compr Canc Netw. 2011. 9:82–113.6. Kim KW, Choi HJ, Kang S, Park SY, Jung DC, Cho JY, et al. The utility of multi-detector computed tomography in the diagnosis of malignant pleural effusion in the patients with ovarian cancer. Eur J Radiol. 2010. 75:230–235.7. Diaz JP, Abu-Rustum NR, Sonoda Y, Downey RJ, Park BJ, Flores RM, et al. Video-assisted thoracic surgery (VATS) evaluation of pleural effusions in patients with newly diagnosed advanced ovarian carcinoma can influence the primary management choice for these patients. Gynecol Oncol. 2010. 116:483–488.8. Munstedt K, Franke FE. Role of primary surgery in advanced ovarian cancer. World J Surg Oncol. 2004. 2:32.9. Huober J, Meyer A, Wagner U, Wallwiener D. The role of neoadjuvant chemotherapy and interval laparotomy in advanced ovarian cancer. J Cancer Res Clin Oncol. 2002. 128:153–160.10. Schwartz PE. Cytoreductive surgery for the management of stage IV ovarian cancer. Gynecol Oncol. 1997. 64:1–3.11. Vergote I, Trope CG, Amant F, Kristensen GB, Ehlen T, Johnson N, et al. Neoadjuvant chemotherapy or primary surgery in stage IIIC or IV ovarian cancer. N Engl J Med. 2010. 363:943–953.12. Eitan R, Levine DA, Abu-Rustum N, Sonoda Y, Huh JN, Franklin CC, et al. The clinical significance of malignant pleural effusions in patients with optimally debulked ovarian carcinoma. Cancer. 2005. 103:1397–1401.13. Juretzka MM, Abu-Rustum NR, Sonoda Y, Downey RJ, Flores RM, Park BJ, et al. The impact of video-assisted thoracic surgery (VATS) in patients with suspected advanced ovarian malignancies and pleural effusions. Gynecol Oncol. 2007. 104:670–674.14. Chi DS, Abu-Rustum NR, Sonoda Y, Chen SW, Flores RM, Downey R, et al. The benefit of video-assisted thoracoscopic surgery before planned abdominal exploration in patients with suspected advanced ovarian cancer and moderate to large pleural effusions. Gynecol Oncol. 2004. 94:307–311.15. Mironov O, Ishill NM, Mironov S, Vargas HA, Zheng J, Moskowitz CS, et al. Pleural effusion detected at CT prior to primary cytoreduction for stage III or IV ovarian carcinoma: effect on survival. Radiology. 2011. 258:776–784.16. Leung AN, Muller NL, Miller RR. CT in differential diagnosis of diffuse pleural disease. AJR Am J Roentgenol. 1990. 154:487–492.17. Traill ZC, Davies RJ, Gleeson FV. Thoracic computed tomography in patients with suspected malignant pleural effusions. Clin Radiol. 2001. 56:193–196.18. Grunze H. The comparative diagnostic accuracy, efficiency and specificity of cytologic technics used in the diagnosis of malignant neoplasm in serous effusions of the pleural and pericardial cavities. Acta Cytol. 1964. 8:150–163.19. Sahn SA. Pleural diseases related to metastatic malignancies. Eur Respir J. 1997. 10:1907–1913.20. Sallach SM, Sallach JA, Vasquez E, Schultz L, Kvale P. Volume of pleural fluid required for diagnosis of pleural malignancy. Chest. 2002. 122:1913–1917.21. Lim MC, Lee HS, Jung DC, Choi JY, Seo SS, Park SY. Pathological diagnosis and cytoreduction of cardiophrenic lymph node and pleural metastasis in ovarian cancer patients using video-assisted thoracic surgery. Ann Surg Oncol. 2009. 16:1990–1996.22. Mergo PJ, Helmberger T, Didovic J, Cernigliaro J, Ros PR, Staab EV. New formula for quantification of pleural effusions from computed tomography. J Thorac Imaging. 1999. 14:122–125.23. du Bois A, Quinn M, Thigpen T, Vermorken J, Avall-Lundqvist E, Bookman M, et al. 2004 consensus statements on the management of ovarian cancer: final document of the 3rd International Gynecologic Cancer Intergroup Ovarian Cancer Consensus Conference (GCIG OCCC 2004). Ann Oncol. 2005. 16:Suppl 8. viii7–viii12.24. van der Burg ME, van Lent M, Buyse M, Kobierska A, Colombo N, Favalli G, et al. The effect of debulking surgery after induction chemotherapy on the prognosis in advanced epithelial ovarian cancer: Gynecological Cancer Cooperative Group of the European Organization for Research and Treatment of Cancer. N Engl J Med. 1995. 332:629–634.25. Bonnefoi H, A'Hern RP, Fisher C, Macfarlane V, Barton D, Blake P, et al. Natural history of stage IV epithelial ovarian cancer. J Clin Oncol. 1999. 17:767–775.26. Penson RT, Skates SJ, Fuller AJ Jr, Seiden MV. Clinical course of stage IV epithelial ovarian cancer. J Clin Oncol. 1999. 17:3361–3362.27. Aletti GD, Podratz KC, Cliby WA, Gostout BS. Stage IV ovarian cancer: disease site-specific rationale for postoperative treatment. Gynecol Oncol. 2009. 112:22–27.28. Eisenkop SM. Thoracoscopy for the management of advanced epithelial ovarian cancer: a preliminary report. Gynecol Oncol. 2002. 84:315–320.29. Bristow RE, Tomacruz RS, Armstrong DK, Trimble EL, Montz FJ. Survival effect of maximal cytoreductive surgery for advanced ovarian carcinoma during the platinum era: a meta-analysis. J Clin Oncol. 2002. 20:1248–1259.30. Munkarah AR, Hallum AV 3rd, Morris M, Burke TW, Levenback C, Atkinson EN, et al. Prognostic significance of residual disease in patients with stage IV epithelial ovarian cancer. Gynecol Oncol. 1997. 64:13–17.31. Cohen-Mouly S, Badia A, Bats AS, Barthes F, Bensaid C, Riquet M, et al. Role of video-assisted thoracoscopy in patients with ovarian cancer and pleural effusion. Int J Gynecol Cancer. 2009. 19:1662–1665.32. Erasmus JJ, McAdams HP, Rossi SE, Goodman PC, Coleman RE, Patz EF. FDG PET of pleural effusions in patients with non-small cell lung cancer. AJR Am J Roentgenol. 2000. 175:245–249.33. Orki A, Akin O, Tasci AE, Ciftci H, Urek S, Falay O, et al. The role of positron emission tomography/computed tomography in the diagnosis of pleural diseases. Thorac Cardiovasc Surg. 2009. 57:217–221.34. Yildirim H, Metintas M, Entok E, Ak G, Ak I, Dundar E, et al. Clinical value of fluorodeoxyglucose-positron emission tomography/computed tomography in differentiation of malignant mesothelioma from asbestos-related benign pleural disease: an observational pilot study. J Thorac Oncol. 2009. 4:1480–1484.35. Kitajima K, Murakami K, Yamasaki E, Kaji Y, Fukasawa I, Inaba N, et al. Diagnostic accuracy of integrated FDG-PET/contrastenhanced CT in staging ovarian cancer: comparison with enhanced CT. Eur J Nucl Med Mol Imaging. 2008. 35:1912–1920.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Video-assisted Thoracic Surgery Lobectomy
- Port Site Metastasis of Breast Cancer after Video-Assisted Thoracic Surgery for Pulmonary Metastasis of Breast Cancer: A Case Report
- Maximal cytoreductive effort in epithelial ovarian cancer surgery
- Azygos Vein Aneurysm: A Case for Elective Resection by Video-assisted Thoracic Surgery
- Video-Assisted Thoracic Surgery Thymectomy: Transpleural Approach