Blood Res.
2014 Sep;49(3):192-195. 10.5045/br.2014.49.3.192.
Hereditary hemorrhagic telangiectasia treated with low dose intravenous bevacizumab
- Affiliations
-
- 1Department of Internal Medicine, Soonchunhyang University Cheonan Hospital, Cheonan, Korea. khy1234@schmc.ac.kr
- KMID: 2172792
- DOI: http://doi.org/10.5045/br.2014.49.3.192
Abstract
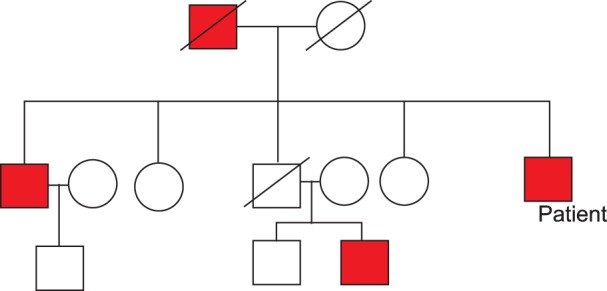
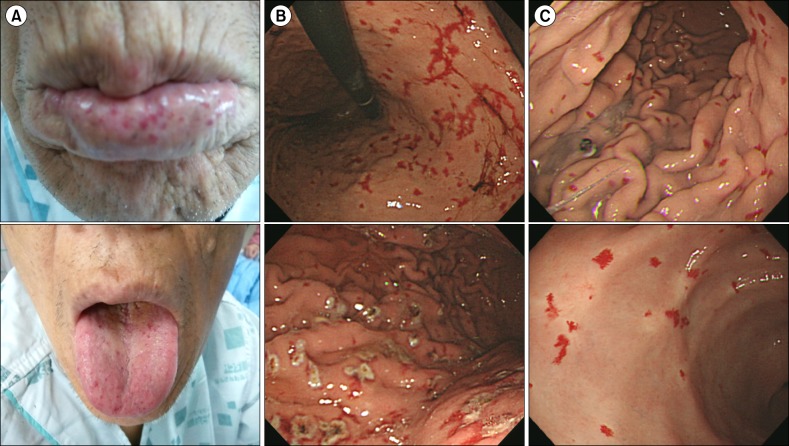
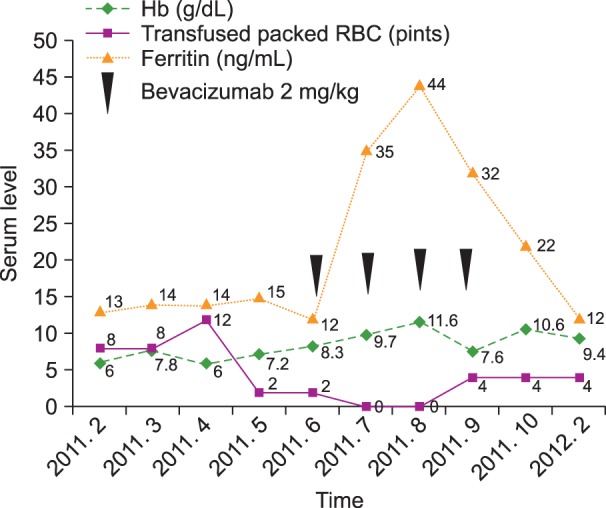
- Hereditary hemorrhagic telangiectasia (HHT) is an autosomal dominant disorder that leads to mucocutaneous telangiectasias, epistaxis, and gastrointestinal bleeding. Depending on the severity and manifestation of the disease, various therapeutic modalities have been used, from local bleeding control to surgery or concomitant drug therapy. Several articles under review have presented guidelines for treatment of HHT with bevacizumab as a direct anti-angiogenesis strategy. Still, neither the exact optimal dose nor the minimum effective dose of intravenous bevacizumab in patients with severe HHT has been reported. A 55-year-old man presented with long-standing epistaxis, recent melena, dizziness, and a three-generation family history of chronic epistaxis, anemia, and regular blood transfusions. Treatment with argon plasma coagulation (APC) for the gastrointestinal bleeding failed to raise hemoglobin levels, we considered using the bevacizumab. We report a patient with severe HHT, who was treated with low-dose bevacizumab (2 mg/kg) and improved substantially.
MeSH Terms
Figure
Reference
-
1. Shovlin CL, Guttmacher AE, Buscarini E, et al. Diagnostic criteria for hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber syndrome). Am J Med Genet. 2000; 91:66–67. PMID: 10751092.
Article2. Shovlin CL. Hereditary haemorrhagic telangiectasia: pathophysiology, diagnosis and treatment. Blood Rev. 2010; 24:203–219. PMID: 20870325.
Article3. Sadick H, Riedel F, Naim R, et al. Patients with hereditary hemorrhagic telangiectasia have increased plasma levels of vascular endothelial growth factor and transforming growth factor-beta1 as well as high ALK1 tissue expression. Haematologica. 2005; 90:818–828. PMID: 15951295.4. Bose P, Holter JL, Selby GB. Bevacizumab in hereditary hemorrhagic telangiectasia. N Engl J Med. 2009; 360:2143–2144. PMID: 19439755.
Article5. Kim YJ, Kim IH, Moon TH, et al. A case of hereditary hemorrhagic telangiectasia with pulmonary arteriovenous malformation. Korean J Med. 1996; 50:571–575.6. Suppressa P, Liso A, Sabba C. Low dose intravenous bevacizumab for the treatment of anaemia in hereditary haemorrhagic telangiectasia. Br J Haematol. 2011; 152:365. PMID: 21265821.7. Richards-Yutz J, Grant K, Chao EC, Walther SE, Ganguly A. Update on molecular diagnosis of hereditary hemorrhagic telangiectasia. Hum Genet. 2010; 128:61–77. PMID: 20414677.
Article8. Amanzada A, Toppler GJ, Cameron S, Schworer H, Ramadori G. A case report of a patient with hereditary hemorrhagic telangiectasia treated successively with thalidomide and bevacizumab. Case Rep Oncol. 2010; 3:463–470. PMID: 21611144.
Article9. Loges S, Roncal C, Carmeliet P. Development of targeted angiogenic medicine. J Thromb Haemost. 2009; 7:21–33. PMID: 18983480.
Article10. Cohen MH, Gootenberg J, Keegan P, Pazdur R. FDA drug approval summary: bevacizumab (Avastin) plus Carboplatin and Paclitaxel as first-line treatment of advanced/metastatic recurrent nonsquamous non-small cell lung cancer. Oncologist. 2007; 12:713–718. PMID: 17602060.
Article11. Lu JF, Bruno R, Eppler S, Novotny W, Lum B, Gaudreault J. Clinical pharmacokinetics of bevacizumab in patients with solid tumors. Cancer Chemother Pharmacol. 2008; 62:779–786. PMID: 18205003.
Article12. Brinkerhoff BT, Poetker DM, Choong NW. Long-term therapy with bevacizumab in hereditary hemorrhagic telangiectasia. N Engl J Med. 2011; 364:688–689. PMID: 21323562.
Article13. Lazaraki G, Akriviadis E, Pilpilidis I, Parisi I, Tzilves D, Tarpangos A. Low dose of bevacizumab is safe and effective in preventing bleeding episodes in hereditary hemorrhagic telangiectasia. Am J Gastroenterol. 2011; 106:2204–2206. PMID: 22138950.
Article14. Fodstad P, Dheyauldeen S, Rinde M, Bachmann-Harildstad G. Anti-VEGF with 3-week intervals is effective on anemia in a patient with severe hereditary hemorrhagic telangiectasia. Ann Hematol. 2011; 90:611–612. PMID: 20824275.
Article15. Rohrmeier C, Kuhnel TS. Bevacizumab in therapy-refractory epistaxis: case report of low-dose antibody therapy for hereditary hemorrhagic telangiectasia. HNO. 2012; 60:1003–1006. PMID: 22706563.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Three Cases of Hereditary Hemorrhagic Telangiectasia Treated with Bevacizumab
- Hereditary Hemorrhagic Telangiectasia Combined with Pulmonary Arteriovenous Malformation Treated with Transcatheter Embolotherapy
- Hereditary Hemorrhagic Telangiectasia in a Family
- A Case of Hereditary Hemorrhagic Telangiectasia
- Genetic Mutation Analysis Can Supplement Clinically Confirmed Hereditary Hemorrhagic Telangiectasia Populations