Chonnam Med J.
2015 Dec;51(3):135-138. 10.4068/cmj.2015.51.3.135.
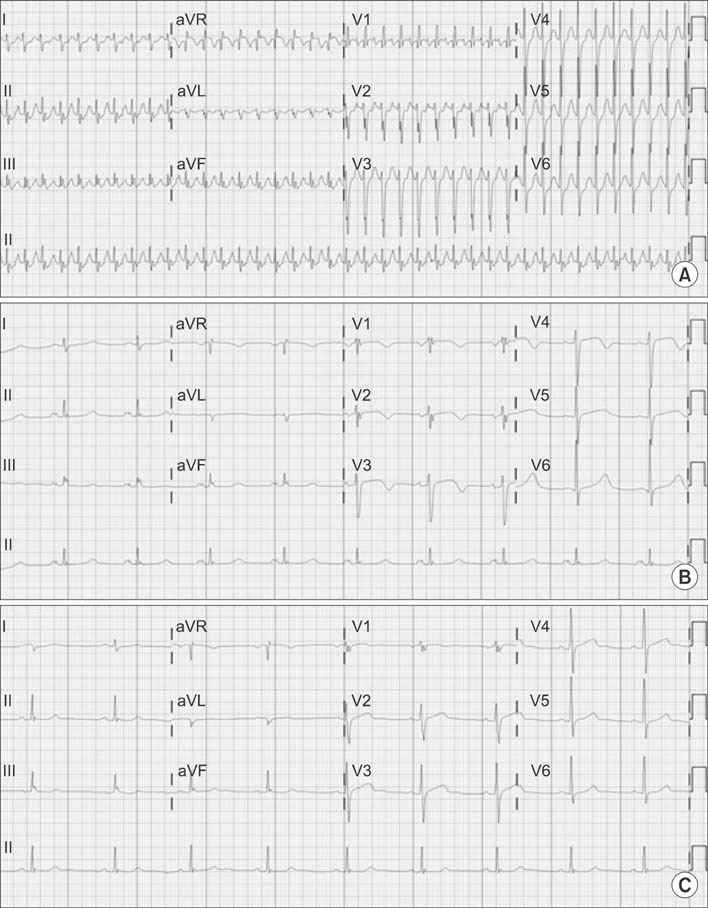
Tachycardia-Induced Right Heart Failure and Severe Tricuspid Regurgitation That Improved with Medication
- Affiliations
-
- 1Department of Internal Medicine, Kyungpook National University School of Medicine, Daegu, Korea. ddhyang@knu.ac.kr
- KMID: 2172130
- DOI: http://doi.org/10.4068/cmj.2015.51.3.135
Abstract
- Secondary tricuspid regurgitation (TR) primarily develops due to left heart failure or primary pulmonary diseases. Tricuspid annular dilation, which is commonly caused by right ventricular volume and pressure overload followed by right ventricle dilation, is believed to be the main mechanism underlying secondary TR. It is reported that once the tricuspid annulus is dilated, its size cannot spontaneously return to normal, and it may continue to dilate. These reports also suggest the use of an aggressive surgical approach for secondary TR. In the present report, we describe a case of tachycardia-induced severe TR that was completely resolved without the need for surgery.
MeSH Terms
Figure
Reference
-
1. The Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC), European Association for Cardio-Thoracic Surgery (EACTS). Vahanian A, Alfieri O, Andreotti F, Antunes MJ, et al. Guidelines on the management of valvular heart disease. Eur Heart J. 2012; 33:2451–2496.2. Yamasaki N, Kondo F, Kubo T, Okawa M, Matsumura Y, Kitaoka H, et al. Severe tricuspid regurgitation in the aged: atrial remodeling associated with long-standing atrial fibrillation. J Cardiol. 2006; 48:315–323.3. Jeong YH, Choi KJ, Song JM, Hwang ES, Park KM, Nam GB, et al. Diagnostic approach and treatment strategy in tachycardia-induced cardiomyopathy. Clin Cardiol. 2008; 31:172–178.
Article4. Gupta S, Figueredo VM. Tachycardia mediated cardiomyopathy: pathophysiology, mechanisms, clinical features and management. Int J Cardiol. 2014; 172:40–46.
Article5. Rogers JH, Bolling SF. The tricuspid valve: current perspective and evolving management of tricuspid regurgitation. Circulation. 2009; 119:2718–2725.6. Lozano HF, Sharma CN. Reversible pulmonary hypertension, tricuspid regurgitation and right-sided heart failure associated with hyperthyroidism: case report and review of the literature. Cardiol Rev. 2004; 12:299–305.
Article7. Taramasso M, Vanermen H, Maisano F, Guidotti A, La Canna G, Alfieri O. The growing clinical importance of secondary tricuspid regurgitation. J Am Coll Cardiol. 2012; 59:703–710.
Article8. Dreyfus GD, Corbi PJ, Chan KM, Bahrami T. Secondary tricuspid regurgitation or dilatation: which should be the criteria for surgical repair? Ann Thorac Surg. 2005; 79:127–132.
Article9. Lee JW, Song JM, Park JP, Lee JW, Kang DH, Song JK. Long-term prognosis of isolated significant tricuspid regurgitation. Circ J. 2010; 74:375–380.
Article10. Koelling TM, Aaronson KD, Cody RJ, Bach DS, Armstrong WF. Prognostic significance of mitral regurgitation and tricuspid regurgitation in patients with left ventricular systolic dysfunction. Am Heart J. 2002; 144:524–529.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reversible severe tricuspid regurgitation with right heart failure associated with thyrotoxicosis
- High Cardiac Output Heart Failure Induced by Chronic Severe Anemia
- Improvement of Severe Tricuspid Regurgitation with Right Heart Failure Associated with Thyrotoxicosis due to Graves' Disease
- A Case of Neonatal Transient Tricuspid Regurgitation with Cardiomegaly in Fetal Period
- Permanent Pacemaker Lead Induced Severe Tricuspid Regurgitation in Patient Undergoing Multiple Valve Surgery