Ann Dermatol.
2009 Feb;21(1):71-74. 10.5021/ad.2009.21.1.71.
Angiolymphoid Hyperplasia with Eosinophilia That Was Possibly Induced by Vaccination in a Child
- Affiliations
-
- 1Department of Dermatology, School of Medicine, Chungnam National University, Daejeon, Korea. jhoon@cnu.ac.kr
- KMID: 2172072
- DOI: http://doi.org/10.5021/ad.2009.21.1.71
Abstract
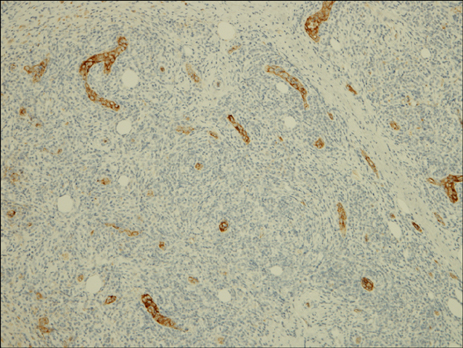
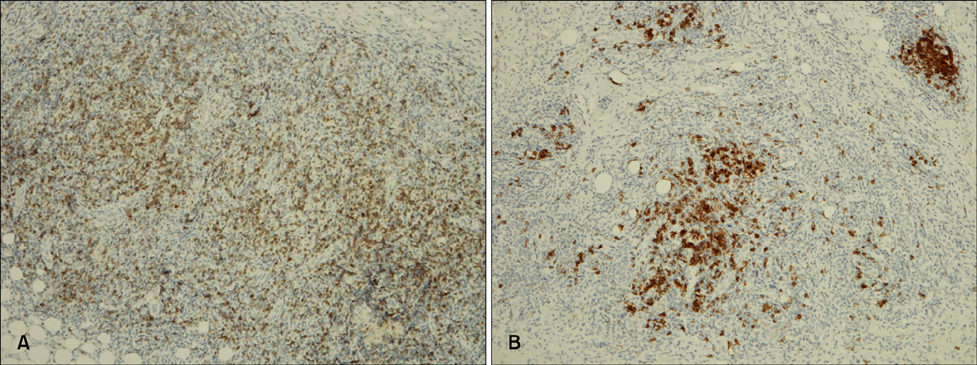
- Angiolymphoid hyperplasia with eosinophilia (ALHE) is a rare benign vasoproliferative disease of an unknown cause involving the skin or subcutaneous tissue of the head and neck, and particularly around the ear. It predominantly affects Caucasian adults during the third and fourth decades and it very rarely occurs in children. We experienced a case of ALHE in a 2-year-old Korean boy who had a firm, pruritic, skin-colored, subcutaneous nodule on his right upper arm. The histopathological findings were compatible with ALHE and they showed prominent vascular changes with epitheloid or histiocytoid endothelial cells surrounded by inflammatory cells, including a large proportion of eosinophils. This unusual distribution of the lesion and the young age of the patient may be associated with vaccination.
MeSH Terms
Figure
Reference
-
1. Wells GC, Whimster IW. Subcutaneous angiolymphoid hyperplasia with eosinophilia. Br J Dermatol. 1969. 81:1–14.
Article2. Kennedy CTC. Champion RH, Burton JL, Burns DA, Breathnach SM, editors. The external ear. Rook/Wilkinson/Ebling textbook of dermatology. 1998. 6th ed. Malden: Blackwell Science;3027–3028.
Article3. Iguchi Y, Inoue T, Shimono M, Yamamura T, Shigematsu T, Takahashi S. Kimura's disease and its relation to angiolymphoid hyperplasia with eosinophilia: report of three cases and review of the literature. J Oral Pathol. 1986. 15:132–137.
Article4. Googe PB, Harris NL, Mihm MC Jr. Kimura's disease and angiolymphoid hyperplasia with eosinophilia: two distinct histopathological entities. J Cutan Pathol. 1987. 14:263–271.
Article5. Mehregan AH, Shapiro L. Angiolymphoid hyperplasia with eosinophilia. Arch Dermatol. 1971. 103:50–57.
Article6. Rosai J, Gold J, Landy R. The histiocytoid hemangiomas. A unifying concept embracing several previously described entities of skin, soft tissue, large vessels, bone, and heart. Hum Pathol. 1979. 10:707–730.7. Urabe A, Tsuneyoshi M, Enjoji M. Epithelioid hemangioma versus Kimura's disease. A comparative clinicopathologic study. Am J Surg Pathol. 1987. 11:758–766.8. Chun SI, Ji HG. Kimura's disease and angiolymphoid hyperplasia with eosinophilia: clinical and histopathologic differences. J Am Acad Dermatol. 1992. 27:954–958.
Article9. Henry PG, Burnett JW. Angiolymphoid hyperplasia with eosinophilia. Arch Dermatol. 1978. 114:1168–1172.
Article10. Olsen TG, Helwig EB. Angiolymphoid hyperplasia with eosinophilia. A clinicopathologic study of 116 patients. J Am Acad Dermatol. 1985. 12:781–796.11. Arnold M, Geilen CC, Coupland SE, Krengel S, Dippel E, Sproder J, et al. Unilateral angiolymphoid hyperplasia with eosinophilia involving the left arm and hand. J Cutan Pathol. 1999. 26:436–440.
Article12. Akosa AB, Ali MH, Khoo CT, Evans DM. Angiolymphoid hyperplasia with eosinophilia associated with tetanus toxoid vaccination. Histopathology. 1990. 16:589–593.
Article13. Hallam LA, Mackinlay GA, Wright AM. Angiolymphoid hyperplasia with eosinophilia: possible aetiological role for immunisation. J Clin Pathol. 1989. 42:944–949.
Article14. Helander SD, Peters MS, Kuo TT, Su WP. Kimura's disease and angiolymphoid hyperplasia with eosinophilia: new observations from immunohistochemical studies of lymphocyte markers, endothelial antigens, and granulocyte proteins. J Cutan Pathol. 1995. 22:319–326.
Article15. Haas AF, La Perriere R, King E. Angiolymphoid hyperplasia with eosinophilia of the hand. A case report. J Dermatol Surg Oncol. 1991. 17:731–734.16. Baum EW, Sams WM Jr, Monheit GD. Angiolymphoid hyperplasia with eosinophilia. The disease and a comparison of treatment modalities. J Dermatol Surg Oncol. 1982. 8:966–970.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Angiolymphoid Hyperplasia with Eosinophilia
- Angiolymphoid Hyperplasia with Eosinophilia in Bone: A Case Report
- A Case of Angiolymphoid Hyperplasia with Eosinophilia
- A Case of Angiolymphoid Hyperplasia with Eosinophilia
- Histiocytoid Hemangioma (Angiolymphoid Hyperplasia with Eosinophilia): Effective Treatment with Dapsone