Ann Dermatol.
2010 Feb;22(1):48-50. 10.5021/ad.2010.22.1.48.
A Case of p-ANCA-Positive Propylthiouracil-Induced Pyoderma Gangrenosum
- Affiliations
-
- 1Department of Dermatology, Maryknoll Medical Center, Busan, Korea. drj715@naver.com
- 2Department of Dermatology, College of Medicine, Inje University, Busan, Korea.
- KMID: 2172036
- DOI: http://doi.org/10.5021/ad.2010.22.1.48
Abstract
- Propylthiouracil is a common medication used in patients with hyperthyroidism; it can cause perinuclear antineutrophil cytoplasmic antibodies (p-ANCA) in some patients with Graves' disease. This antibody has been associated with various forms of vasculitis and neutrophilic dermatosis. Herein, we report a patient who presented with cutaneous manifestations of pyoderma gangrenosum with simultaneous development of p-ANCAs during PTU therapy for Graves' disease.
Keyword
MeSH Terms
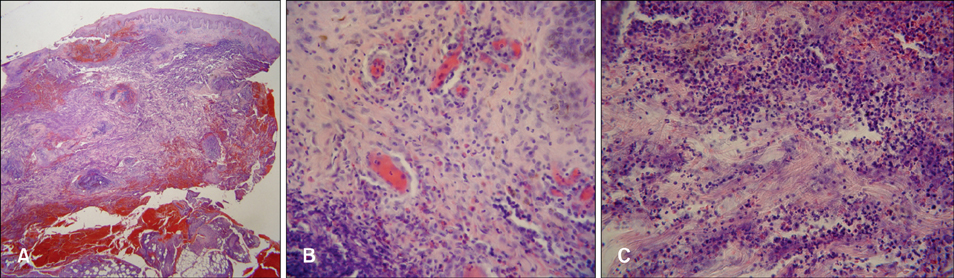
Figure
Cited by 1 articles
-
A Case of Propylthiouracil induced Antineutrophil Cytoplasmic Antibody Positive Pyoderma Gangrenosum
Ji Yeon Lee, Ji Min Lee, Tae Han Lee, Hye Jin Jeong, Go Choi, Jin Nyeong Chae, Ji-Min Kim, Sang-Hyon Kim
J Rheum Dis. 2014;21(3):162-165. doi: 10.4078/jrd.2014.21.3.162.
Reference
-
1. Darben T, Savige J, Prentice R, Paspaliaris B, Chick J. Pyoderma gangrenosum with secondary pyarthrosis following propylthiouracil. Australas J Dermatol. 1999. 40:144–146.
Article2. Miller RM, Darben TA, Nedwich J, Savige J. Propylthiouracil-induced antineutrophil cytoplasmic antibodies in a patient with Graves' disease and a neutrophilic dermatosis. Br J Dermatol. 1999. 141:943–944.
Article3. Hong SB, Lee MH. A case of propylthiouracil-induced pyoderma gangrenosum associated with antineutrophil cytoplasmic antibody. Dermatology. 2004. 208:339–341.
Article4. Gungor K, Gonen S, Kisakol G, Dikbas O, Kaya A. ANCA positive propylthiouracil induced pyoderma gangrenosum. J Endocrinol Invest. 2006. 29:575–576.
Article5. Jacobs EM, Hartkamp A, Kaasjager HA. PTU-associated cutaneous vasculitis with ANCA anti-MPO and anti-PR3 antibodies. Neth J Med. 2003. 61:296–299.6. Sato H, Hattori M, Fujieda M, Sugihara S, Inomata H, Hoshi M, et al. High prevalence of antineutrophil cytoplasmic antibody positivity in childhood onset Graves' disease treated with propylthiouracil. J Clin Endocrinol Metab. 2000. 85:4270–4273.
Article7. Kitahara T, Hiromura K, Maezawa A, Ono K, Narabara N, Yano S, et al. Case of propylthiouracil-induced vasculitis associated with anti-neutrophil cytoplasmic antibody (ANCA); review of literature. Clin Nephrol. 1997. 47:336–340.8. Miller RM, Savige J, Nassis L, Cominos BI. Antineutrophil cytoplasmic antibody (ANCA)-positive cutaneous leucocytoclastic vasculitis associated with antithyroid therapy in Graves' disease. Australas J Dermatol. 1998. 39:96–99.
Article9. Wang LH, Tsai MJ, Tsai WY, Lee JS, Chiang BL. Propylthiouracil-induced antineutrophil cytoplasm antibody-positive anaphylactoid purpura-like vasculitis--a case report. J Formos Med Assoc. 2000. 99:642–645.10. Sheen YS, Chu CY, Yu HS. Antineutrophil cytoplasmic antibody-positive cutaneous leukocytoclastic vasculitis associated with propylthiouracil therapy. Arch Dermatol. 2006. 142:879–880.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Propylthiouracil induced Antineutrophil Cytoplasmic Antibody Positive Pyoderma Gangrenosum
- A Case of Behcet's Disease Associated with Pyoderma Gangrenosum
- A Case of Pyoderma Gangrenosum Occurring in Behcet's Disease
- A Case of Post-traumatic Pyoderma Gangrenosum Associated with Ulcerative Colitis
- A Case of Pyoderma Gangrenosum Associated with Acute Leukemia