Endocrinol Metab.
2015 Dec;30(4):481-487. 10.3803/EnM.2015.30.4.481.
A 5-Year Prospective Follow-Up Study of Lipid-Rich Adrenal Incidentalomas: No Tumor Growth or Development of Hormonal Hypersecretion
- Affiliations
-
- 1Department of Endocrinology, Abdominal Center, Helsinki University Central Hospital, University of Helsinki, Helsinki, Finland. camilla.schalin-jantti@hus.fi
- 2Department of Radiology, HUS Medical Imaging Center, Helsinki University Central Hospital, University of Helsinki, Helsinki, Finland.
- 3HUSLAB, Department of Clinical Chemistry, University of Helsinki, Helsinki, Finland.
- KMID: 2169656
- DOI: http://doi.org/10.3803/EnM.2015.30.4.481
Abstract
- BACKGROUND
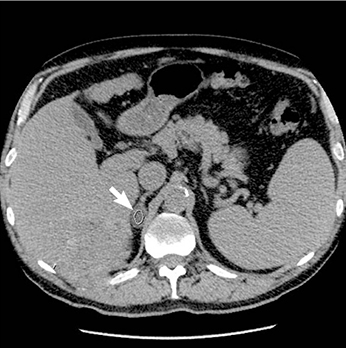
Current guidelines for follow-up of adrenal incidentalomas are extensive and hampered by lack of follow-up studies. We tested the hypothesis that small lipid-rich adrenal incidentalomas, initially characterized by tumor size <40 mm and <10 Hounsfield units (HUs) on unenhanced computed tomography (CT) may not demonstrate excessive growth/hormonal hypersecretion on follow-up.
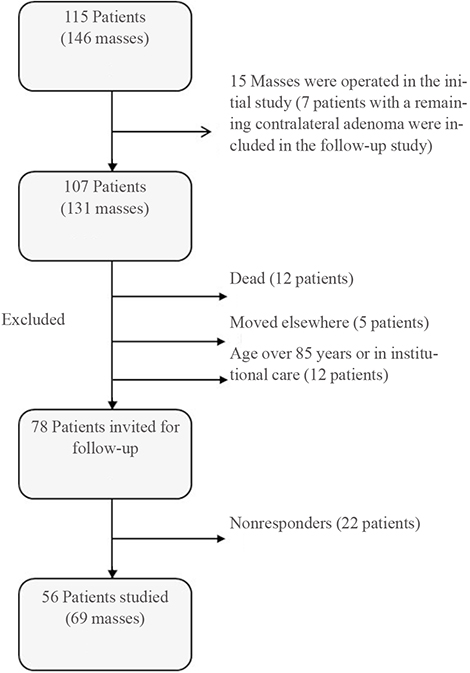
METHODS
Sixty-nine incidentalomas in 56 patients were restudied with unenhanced CT and screening for hypercortisolism (dexamethasone suppression test [DST], plasma adrenocorticotropic hormone) and pheochromocytoma (24-hour urinary metanephrines and normetanephrines) 5 years later. Primary hyperaldosteronism was excluded at base-line.
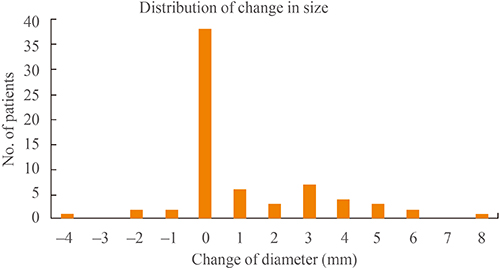
RESULTS
Tumor (n=69) size was similar before and after 5 years follow-up (19+/-6 mm vs. 20+/-7 mm). Mean tumor growth was 1+/-2 mm. Largest increase in tumor size was 8 mm, this tumor was surgically removed and histopathology confirmed cortical adenoma. DST was normal in 54 patients and two patients (3.6%) were still characterized by subclinical hypercortisolism. Initial tumor size was >20 mm for the patient with largest tumor growth and those with subclinical hypercortisolism. All patients had normal 24-hour urinary metanephrines and normetanephrines. Low attenuation (<10 HU) was demonstrated in 97% of 67 masses re-evaluated with unenhanced CT.
CONCLUSION
None of the patients developed clinically relevant tumor growth or new subclinical hypercortisolism. Biochemical screening for pheochromocytoma in incidentalomas demonstrating <10 HU on unenhanced CT is not needed. For such incidentalomas <40 mm, it seems sufficient to perform control CT and screen for hypercortisolism after 5 years.
Keyword
MeSH Terms
Figure
Reference
-
1. Bulow B, Ahren B. Swedish Research Council Study Group of Endocrine Abdominal Tumours. Adrenal incidentaloma: experience of a standardized diagnostic programme in the Swedish prospective study. J Intern Med. 2002; 252:239–246.2. Barzon L, Sonino N, Fallo F, Palu G, Boscaro M. Prevalence and natural history of adrenal incidentalomas. Eur J Endocrinol. 2003; 149:273–285.3. Young WF Jr. Clinical practice: the incidentally discovered adrenal mass. N Engl J Med. 2007; 356:601–610.4. Terzolo M, Bovio S, Pia A, Reimondo G, Angeli A. Management of adrenal incidentaloma. Best Pract Res Clin Endocrinol Metab. 2009; 23:233–243.5. Zeiger MA, Siegelman SS, Hamrahian AH. Medical and surgical evaluation and treatment of adrenal incidentalomas. J Clin Endocrinol Metab. 2011; 96:2004–2015.6. Terzolo M, Stigliano A, Chiodini I, Loli P, Furlani L, Arnaldi G, et al. AME position statement on adrenal incidentaloma. Eur J Endocrinol. 2011; 164:851–870.7. Grumbach MM, Biller BM, Braunstein GD, Campbell KK, Carney JA, Godley PA, et al. Management of the clinically inapparent adrenal mass ("incidentaloma"). Ann Intern Med. 2003; 138:424–429.8. Thompson GB, Young WF Jr. Adrenal incidentaloma. Curr Opin Oncol. 2003; 15:84–90.9. Nieman LK. Approach to the patient with an adrenal incidentaloma. J Clin Endocrinol Metab. 2010; 95:4106–4113.10. Sane T, Schalin-Jantti C, Raade M. Is biochemical screening for pheochromocytoma in adrenal incidentalomas expressing low unenhanced attenuation on computed tomography necessary? J Clin Endocrinol Metab. 2012; 97:2077–2083.11. Morelli V, Reimondo G, Giordano R, Della Casa S, Policola C, Palmieri S, et al. Long-term follow-up in adrenal incidentalomas: an Italian multicenter study. J Clin Endocrinol Metab. 2014; 99:827–834.12. Tabarin A, Bardet S, Bertherat J, Dupas B, Chabre O, Hamoir E, et al. Exploration and management of adrenal incidentalomas. French Society of Endocrinology Consensus. Ann Endocrinol (Paris). 2008; 69:487–500.13. Zeiger MA, Thompson GB, Duh QY, Hamrahian AH, Angelos P, Elaraj D, et al. The American Association of Clinical Endocrinologists and American Association of Endocrine Surgeons medical guidelines for the management of adrenal incidentalomas. Endocr Pract. 2009; 15:Suppl 1. 1–20.14. Arnaldi G, Boscaro M. Adrenal incidentaloma. Best Pract Res Clin Endocrinol Metab. 2012; 26:405–419.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Is Follow-up of Adrenal Incidentalomas Always Mandatory?
- A Case of Bilateral Adrenal Myelolipomas with Congenital Adrenal Hyperplasia
- Adrenal Incidentaloma: Imaging Approach and Differential Diagnosis
- A Clinical Study of 11 Cases of Adrenal Ineidentaloma
- A Case of Black Adrenocortical Adenoma Causing Cushing's Syndrome with Contralateral Nonfuncioning Adenoma