Cancer Res Treat.
2004 Dec;36(6):377-383.
An Analysis of the Risk Factors and Management of Lymphocele after Pelvic Lymphadenectomy in Patients with Gynecologic Malignancies
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Yonsei University College of Medicine, Seoul, Korea. shkim70@yumc.yonsei.ac.kr
- 2Institute of Women's Life Science, Yonsei University College of Medicine, Seoul, Korea.
- 3BK-21 Project for Medical Science, Yonsei University College of Medicine, Seoul, Korea.
Abstract
OBJECTIVES
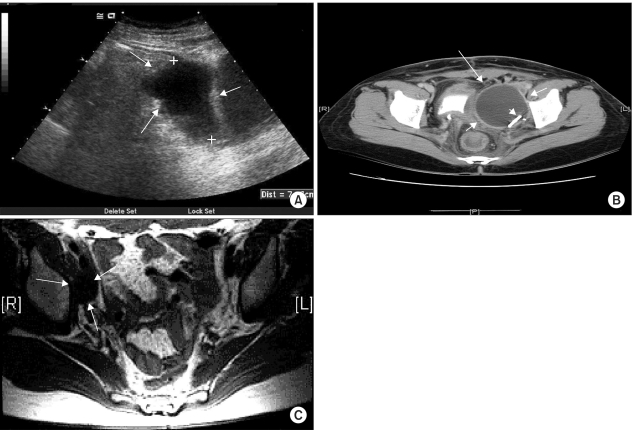
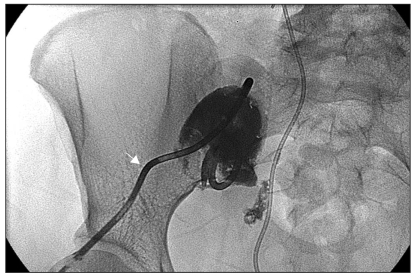
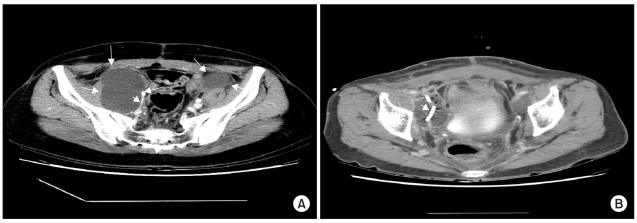
The incidence and risk factors of lymphocele development after pelvic lymphadenectomy were evaluated and its management investigated. MATERIALS AND METHODS: This retrospective study was carried out on 264 patients who received a pelvic lymphadenectomy, between March 1999 and February 2003, due to gynecologic cancer. The patients were classified into two groups; the lymphocele (n=50) and non-lymphocele groups (n=214), as confirmed by ultrasonography, CT scan and MRI. Each group was compared by cancer type and stage, BMI, preoperative Hb, use of pre/postoperative chemotherapy or radiotherapy, number of resected pelvic lymph nodes and the volume of postoperative drainage from a Hemovac(R) pelvic drain. RESULTS: Of the 264 patients tested, 15 of 105 cervical cancer (14%), 22 of 115 ovarian cancer (19%) and 11 of 40 endometrial cancer patients (27%), a total of 50 patients (18%), developed lymphoceles. In the lymphocele group (n=50), 13 patients were diagnosed with complicated lymphocele. The BMI and number of resected pelvic lymph nodes were found to be higher in the lymphocele than in the non-lymphocele group (23.94+/-3.38 vs. 22.52+/-3.00, p=0.00 and 26.80+/-14.82 vs. 22.96+/-10.18, p=0.03, respectively), and showed statistical significance. The occurrence of lymphoceles was lower without postoperative radiotherapy (p=0.01). CONCLUSION: Among the 264 patients, a total of 50 patients (18%) developed lymphoceles. The BMI and number of resected lymph nodes were higher in the lymphocele group, and the use of postoperative radiotherapy was associated with a higher risk of lymphoceles. Thirteen of the 50 patients that developed lymphoceles (n=50) required treatment for lymphocele-related complications.
Keyword
MeSH Terms
Figure
Reference
-
1. Mori N. Clinical and experimental studies on the so-called lymphocyst which develops after radical hysterectomy in cancer of the uterine cervix. J Jpn Obstet Gynecol Soc. 1955; 2:178–203. PMID: 13286539.2. Ilancheran A, Monaghan JM. Pelvic lymphocyst--a 10-year experience. Gynecol Oncol. 1988; 29:333–336. PMID: 3345953.
Article3. Conte M, Panici PB, Guariglia L, Scambia G, Greggi S, Mancuso S. Pelvic lymphocele following radical para-aortic and pelvic lymphadenectomy for cervical carcinoma: incidence rate and percutaneous management. Obstet Gynecol. 1990; 76:268–271. PMID: 2196500.4. Logmans A, Kruyt RH, de Bruin HG, Cox PH, Pillay M, Trimbos JB. Lymphedema and lymphocysts following lymphadenectomy may be prevented by omentoplasty: A pilot study. Gynecol Oncol. 1999; 75:323–327. PMID: 10600283.
Article5. Benedetti-Panici P, Maneschi F, Cutillo G. Pelvic and aortic lymphadenectomy. Surg Clin North Am. 2001; 81:841–858. PMID: 11551129.
Article6. Shingleton HM, Orr HW. Cancer of the cervix: Diagnosis and Treatment in Current reviews in obstetrics and gynecology. 1993. Vol. 5. Edinburgh: Churchill Livingstone.7. Symmonds RE, Pratt JH. Prevention of fistulas and lymphocysts in radical hysterectomy. Preliminary report of a new technic. Obstet Gynecol. 1961; 17:57–64. PMID: 13774382.8. Catalona WJ, Kadmon D, Crane DB. Effect of mini-dose heparin on lymphocele formation following extraperitoneal pelvic lymphadenectomy. J Urol. 1980; 123:890–892. PMID: 7382008.
Article9. Rutledge F, Dodd GD Jr, Kasilag FB Jr. Lymphocysts; a complication of radical pelvic surgery. Am J Obstet Gynecol. 1959; 77:1165–1175. PMID: 13649788.
Article10. Pennehouat G, Mosseri V, Durand JC, Hamelin JP, Asselain B, Pilleron JP, et al. Lymphoceles and peritonization following lymphadenectomy for cancer of the uterus. J Gynecol Obstet Biol Reprod (Paris). 1988; 17:373–378. PMID: 3294282.11. Clarke-Pearson DL, Jelovsek FR, Creasman WT. Thromboembolism complicating surgery for cervical and uterine malignancy: incidence, risk factors, and prophylaxis. Obstet Gynecol. 1983; 61:87–94. PMID: 6823353.12. Orr JW Jr, Barter JF, Kilgore LC, Soong SJ, Shingleton HM, Hatch KD. Closed suction pelvic drainage after radical pelvic surgical procedures. Am J Obstet Gynecol. 1986; 155:867–871. PMID: 3766643.
Article13. White M, Mueller PR, Ferrucci JT Jr, Butch RJ, Simeone JF, Neff CC, et al. Percutaneous drainage of postoperative abdominal and pelvic lymphoceles. AJR Am J Roentgenol. 1985; 145:1065–1069. PMID: 3901705.
Article14. Benedetti-Panici P, Maneschi F, Scambia G, Mancuso S. A new transabdominal approach to the left retroperitoneum for systematic removal of lymph nodes left of the aorta in gynecologic malignancies. Obstet Gynecol. 1994; 83:1060–1064. PMID: 8190424.
Article15. Metcalf KS, Peel KR. Lymphocele. Ann R Coll Surg Engl. 1993; 75:387–392. PMID: 8285540.16. Blebea J, Choudry R. Thigh isosulfan blue injection in the treatment of postoperative lymphatic complications. J Vasc Surg. 1999; 30:350–354. PMID: 10436456.
Article17. Petru E, Tamussino K, Lahousen M, Winter R, Pickel H, Haas J. Pelvic and paraaortic lymphocysts after radical surgery because of cervical and ovarian cancer. Am J Obstet Gynecol. 1989; 161:937–941. PMID: 2801842.
Article18. Livingston WD, Confer DJ, Smith RB. Large lymphoceles resulting from retroperitoneal lymphadenectomy. J Urol. 1980; 124:543–546. PMID: 7420600.
Article19. Spiegel RA, Hessel SJ, Katz ER, Levy JM. Pelvic fullness, urgency and frequency following lymphadenectomy. Pelvic lymphocele. West J Med. 1987; 147:357–358. PMID: 3673073.20. Terada KY, Roberts JA. Lymphoceles following second-look laparotomy for ovarian cancer. Gynecol Oncol. 1988; 29:382–384. PMID: 3345957.
Article21. Benedet JL, Turko M, Boyes DA, Nickerson KG, Bienkowska BT. Radical hysterectomy in the treatment of cervical cancer. Am J Obstet Gynecol. 1980; 137:254–262. PMID: 7377245.
Article22. Nelson JH Jr, HUston JW. Lymphocyst formation following pelvic lymphadenectomy. Am J Obstet Gynecol. 1959; 78:1298–1300. PMID: 14426460.
Article23. de Roo T. The value of lymphography in lymphedema. Surg Gynecol Obstet. 1967; 124:755–765. PMID: 6019288.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Distribution of lymphocele following lymphadenectomy in patients with gynecological malignancies
- Prevention of lymphocele development in gynecologic cancers by the electrothermal bipolar vessel sealing device
- Nomogram predicting risk of lymphocele in gynecologic cancer patients undergoing pelvic lymph node dissection
- Prevention of lymphocele by using gelatin-thrombin matrix as a tissue sealant after pelvic lymphadenectomy in patients with gynecologic cancers: a prospective randomized controlled study
- Laparoscopic pelvic and para-aortic lymphadenectomy