Ann Rehabil Med.
2014 Jun;38(3):304-309. 10.5535/arm.2014.38.3.304.
Effect of the Order of Test Diets on the Accuracy and Safety of Swallowing Studies
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University College of Medicine, Seoul National University Boramae Medical Center, Seoul, Korea. shiuk.lee@gmail.com
- KMID: 2165746
- DOI: http://doi.org/10.5535/arm.2014.38.3.304
Abstract
OBJECTIVE
To assess whether the order of test diets influences the results of swallowing studies with regard to their accuracy and safety.
METHODS
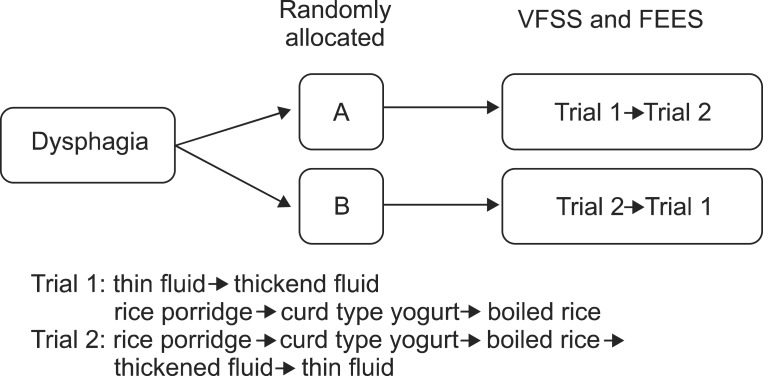
Subjects with suspected dysphagia underwent a videofluoroscopic swallowing study (VFSS) and/or a fiberoptic endoscopic evaluation of swallowing (FEES) and repeated the study on the same day or within a week. The order of test diets comprised of two different sets: trial 1 with the fluid first and trial 2 with the semi-solid food first. Main outcome measurements were the modified penetration-aspiration scale (mPAS) and the pharyngeal residue severity scale (PRSS) for the vallecula and the pyriform sinus.
RESULTS
Sixty-six patients (44 men and 22 women, aged 65.0+/-15.0 years) were enrolled in this study. Forty-three subjects were evaluated with VFSS only and 23 with both VFSS and FEES. As a result of the swallowing studies, there was no significant difference in each chosen diet sequence regarding mPAS and PRSS. Furthermore, there was no difference regarding the duration of studies, rate of premature study termination, rate of abnormal findings in post-study chest X-ray, and rate of fever or pneumonia post-study.
CONCLUSION
The accuracy and safety of the swallowing studies do not rely on the order of test diets.
Keyword
MeSH Terms
Figure
Reference
-
1. Langmore SE, Schatz K, Olsen N. Fiberoptic endoscopic examination of swallowing safety: a new procedure. Dysphagia. 1988; 2:216–219. PMID: 3251697.
Article2. Hiss SG, Postma GN. Fiberoptic endoscopic evaluation of swallowing. Laryngoscope. 2003; 113:1386–1393. PMID: 12897564.
Article3. Jung SH, Lee KJ, Hong JB, Han TR. Validation of clinical dysphagia scale: based on videofluoroscopic swallowing study. J Korean Acad Rehabil Med. 2005; 29:343–350.4. Bingjie L, Tong Z, Xinting S, Jianmin X, Guijun J. Quantitative videofluoroscopic analysis of penetration-aspiration in post-stroke patients. Neurol India. 2010; 58:42–47. PMID: 20228462.
Article5. Han TR, Paik NJ, Park JW. Quantifying swallowing function after stroke: a functional dysphagia scale based on videofluoroscopic studies. Arch Phys Med Rehabil. 2001; 82:677–682. PMID: 11346847.
Article6. Paik NJ, Kim IS, Kim JH, Oh BM, Han TR. Clinical validity of the functional dysphagia scale based on videofluoroscopic swallowing study. J Korean Acad Rehabil Med. 2005; 29:43–49.7. Mann G, Hankey GJ, Cameron D. Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke. 1999; 30:744–748. PMID: 10187872.8. Ott DJ, Pikna LA. Clinical and videofluoroscopic evaluation of swallowing disorders. AJR Am J Roentgenol. 1993; 161:507–513. PMID: 8352094.
Article9. Palmer JB, Kuhlemeier KV, Tippett DC, Lynch C. A protocol for the videofluorographic swallowing study. Dysphagia. 1993; 8:209–214. PMID: 8359040.
Article10. Nishiwaki K, Tsuji T, Liu M, Hase K, Tanaka N, Fujiwara T. Identification of a simple screening tool for dysphagia in patients with stroke using factor analysis of multiple dysphagia variables. J Rehabil Med. 2005; 37:247–251. PMID: 16024482.
Article11. Han TR, Paik NJ, Park JW, Kwon BS. The prediction of persistent dysphagia beyond six months after stroke. Dysphagia. 2008; 23:59–64. PMID: 17602263.
Article12. Logemann JA. Evaluation and treatment of swallowing disorders. San Diego: College Hill Press;1998.13. Paik NJ, Han TR, Park JW, Lee EK, Park MS, Hwang IK. Categorization of dysphagia diets with the line spread test. Arch Phys Med Rehabil. 2004; 85:857–861. PMID: 15129413.14. Li M, Brasseur JG, Kern MK, Dodds WJ. Viscosity measurements of barium sulfate mixtures for use in motility studies of the pharynx and esophagus. Dysphagia. 1992; 7:17–30. PMID: 1424824.
Article15. Clave P, de Kraa M, Arreola V, Girvent M, Farre R, Palomera E, et al. The effect of bolus viscosity on swallowing function in neurogenic dysphagia. Aliment Pharmacol Ther. 2006; 24:1385–1394. PMID: 17059520.
Article16. Goulding R, Bakheit AM. Evaluation of the benefits of monitoring fluid thickness in the dietary management of dysphagic stroke patients. Clin Rehabil. 2000; 14:119–124. PMID: 10763787.17. American Speech-Language-Hearing Association. National Outcomes Measurement System. Adult speech-language pathology training manual. Rockville: American Speech-Language-Hearing Association;1998.18. Han TR, Paik NJ, Park JW. The clinical functional scale for dysphagia in stroke patients. Korean J Stroke. 2001; 3:153–157.19. Chun SW, Lee SA, Jung IY, Beom J, Han TR, Oh BM. Inter-rater agreement for the clinical dysphagia scale. Ann Rehabil Med. 2011; 35:470–476. PMID: 22506161.
Article20. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996; 11:93–98. PMID: 8721066.
Article21. Kim JY, Koh ES, Kim HR, Chun SM, Lee SU, Jung SH. The diagnostic usefulness of the fiberoptic endoscopic evaluation of swallowing. J Korean Acad Rehabil Med. 2011; 35:14–22.22. Kelly AM, Leslie P, Beale T, Payten C, Drinnan MJ. Fibreoptic endoscopic evaluation of swallowing and videofluoroscopy: does examination type influence perception of pharyngeal residue severity? Clin Otolaryngol. 2006; 31:425–432. PMID: 17014453.
Article23. Holas MA, DePippo KL, Reding MJ. Aspiration and relative risk of medical complications following stroke. Arch Neurol. 1994; 51:1051–1053. PMID: 7945003.
Article24. Logemann JA. A manual for videofluoroscopic evaluation of swallowing. 2nd ed. Austin: Pro-Ed;1993.25. Langmore SE. Why I like the free water protocol? Perspect Swallowing Swallowing Disord (Dysphagia). 2011; 20:116–120.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Utility of the Bedside Swallowing Evaluations for Dysphagia
- Overview of the Process of Conducting Meta-analyses of the Diagnostic Test Accuracy
- Effectiveness and safety of low-carbohydrate diets
- Considerations and Problems in the Prescription of Dysphagia Diets
- The Effect of SBAR Communication on Nurse's Perception about Communication and Attitudes toward Patient Safety