Ann Rehabil Med.
2015 Dec;39(6):931-940. 10.5535/arm.2015.39.6.931.
Validity of Quantitative Lymphoscintigraphy as a Lymphedema Assessment Tool for Patients With Breast Cancer
- Affiliations
-
- 1Department of Rehabilitation Medicine, Kyungpook National University College of Medicine, Daegu, Korea. teeed0522@hanmail.net
- 2Department of Rehabilitation Medicine, Kyungpook National University Hospital, Daegu, Korea.
- 3Department of Nuclear Medicine, Kyungpook National University Medical Center, Daegu, Korea.
- 4Department of Surgery, Breast Cancer Center, Kyungpook National University Medical Center, Daegu, Korea.
- KMID: 2165619
- DOI: http://doi.org/10.5535/arm.2015.39.6.931
Abstract
OBJECTIVE
To evaluate the validity of quantitative lymphoscintigraphy as a useful lymphedema assessment tool for patients with breast cancer surgery including axillary lymph node dissection (ALND).
METHODS
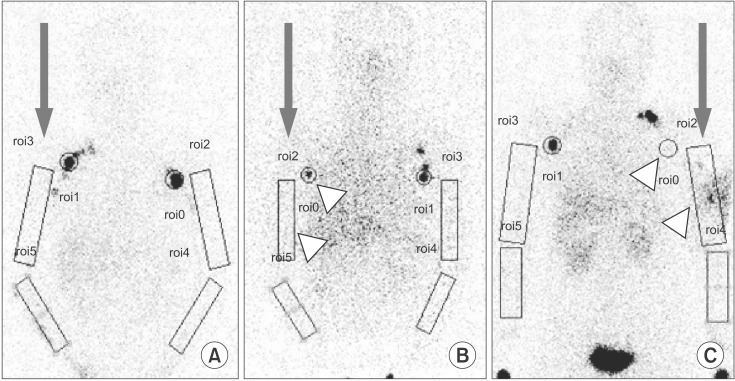
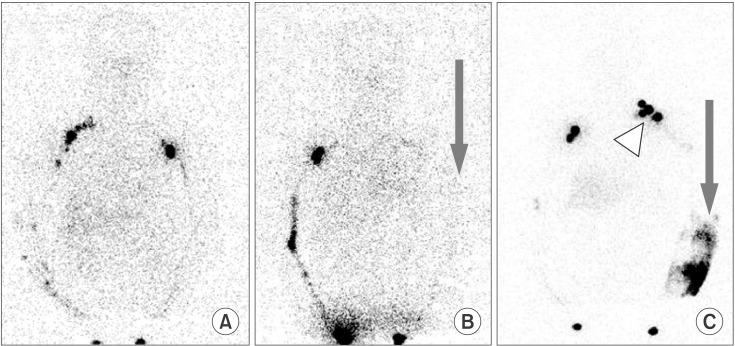
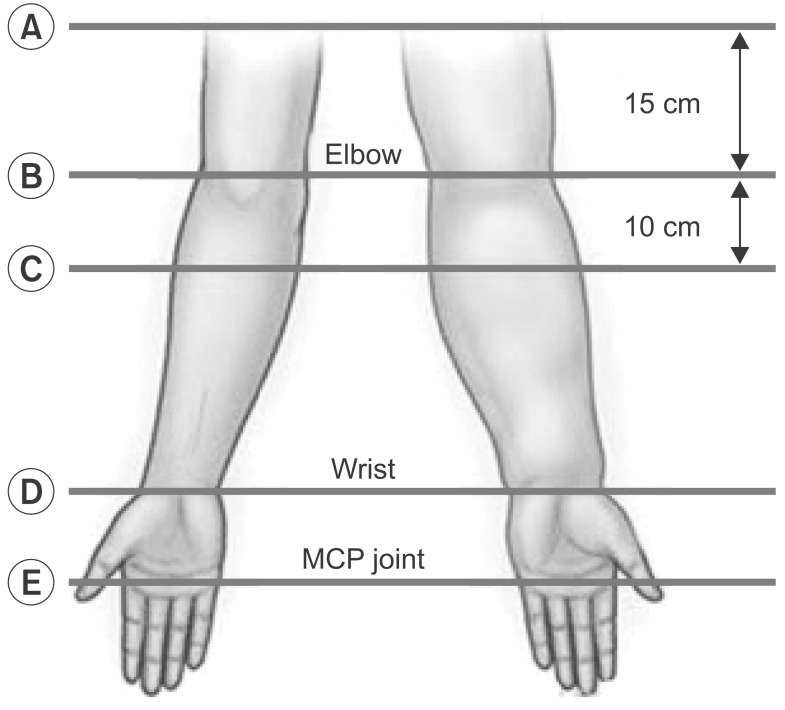
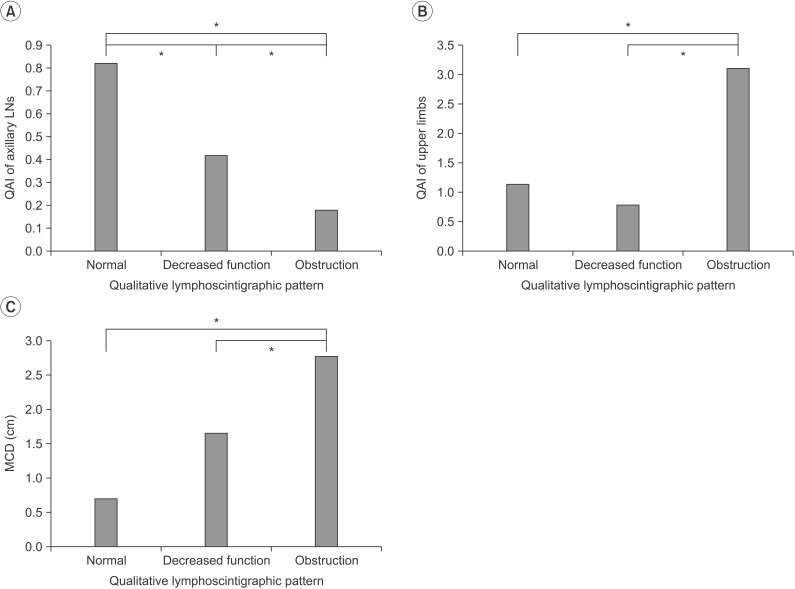
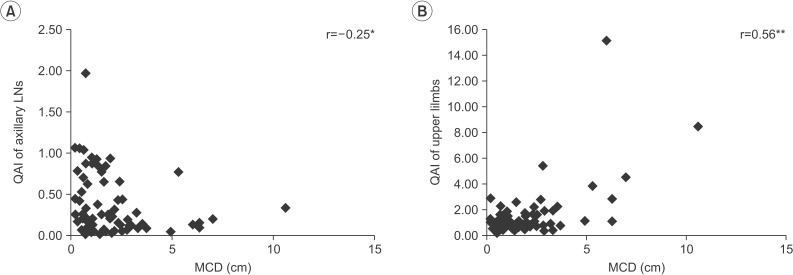
We recruited 72 patients with lymphedema after breast cancer surgery that included ALND. Circumferences in their upper limbs were measured in five areas: 15 cm proximal to the lateral epicondyle (LE), the elbow, 10 cm distal to the LE, the wrist, and the metacarpophalangeal joint. Then, maximal circumference difference (MCD) was calculated by subtracting the unaffected side from the affected side. Quantitative asymmetry indices (QAI) were defined as the radiopharmaceutical uptake ratios of the affected side to the unaffected side. Patients were divided into 3 groups by qualitative lymphoscintigraphic patterns: normal, decreased function, and obstruction.
RESULTS
The MCD was highest in the qualitative obstruction (2.76+/-2.48) pattern with significant differences from the normal (0.69+/-0.78) and decreased function (1.65+/-1.17) patterns. The QAIs of the axillary LNs showed significant differences among the normal (0.82+/-0.29), decreased function (0.42+/-0.41), and obstruction (0.18+/-0.16) patterns. As the QAI of the axillary LN increased, the MCD decreased. The QAIs of the upper limbs were significantly higher in the obstruction (3.12+/-3.07) pattern compared with the normal (1.15+/-0.10) and decreased function (0.79+/-0.30) patterns.
CONCLUSION
Quantitative lymphoscintigraphic analysis is well correlated with both commonly used qualitative lymphoscintigraphic analysis and circumference differences in the upper limbs of patients with breast cancer surgery with ALND. Quantitative lymphoscintigraphy may be a good alternative assessment tool for diagnosing lymphedema after breast cancer surgery with ALND.
MeSH Terms
Figure
Reference
-
1. Deo SV, Ray S, Rath GK, Shukla NK, Kar M, Asthana S, et al. Prevalence and risk factors for development of lymphedema following breast cancer treatment. Indian J Cancer. 2004; 41:8–12. PMID: 15105573.2. Warren AG, Brorson H, Borud LJ, Slavin SA. Lymphedema: a comprehensive review. Ann Plast Surg. 2007; 59:464–472. PMID: 17901744.3. McLaughlin SA, Wright MJ, Morris KT, Giron GL, Sampson MR, Brockway JP, et al. Prevalence of lymphedema in women with breast cancer 5 years after sentinel lymph node biopsy or axillary dissection: objective measurements. J Clin Oncol. 2008; 26:5213–5219. PMID: 18838709.
Article4. Tiwari A, Cheng KS, Button M, Myint F, Hamilton G. Differential diagnosis, investigation, and current treatment of lower limb lymphedema. Arch Surg. 2003; 138:152–161. PMID: 12578410.
Article5. Bar Ad V, Cheville A, Solin LJ, Dutta P, Both S, Harris EE. Time course of mild arm lymphedema after breast conservation treatment for early-stage breast cancer. Int J Radiat Oncol Biol Phys. 2010; 76:85–90. PMID: 19427748.
Article6. Hwang JM, Hwang JH, Kim TW, Lee SY, Chang HJ, Chu IH. Long-term effects of complex decongestive therapy in breast cancer patients with arm lymphedema after axillary dissection. Ann Rehabil Med. 2013; 37:690–697. PMID: 24236257.
Article7. Johansson K, Holmstrom H, Nilsson I, Ingvar C, Albertsson M, Ekdahl C. Breast cancer patients' experiences of lymphoedema. Scand J Caring Sci. 2003; 17:35–42. PMID: 12581293.
Article8. Rietman JS, Dijkstra PU, Geertzen JH, Baas P, de Vries J, Dolsma WV, et al. Treatment-related upper limb morbidity 1 year after sentinel lymph node biopsy or axillary lymph node dissection for stage I or II breast cancer. Ann Surg Oncol. 2004; 11:1018–1024. PMID: 15525832.
Article9. Norman SA, Localio AR, Potashnik SL, Simoes Torpey HA, Kallan MJ, Weber AL, et al. Lymphedema in breast cancer survivors: incidence, degree, time course, treatment, and symptoms. J Clin Oncol. 2009; 27:390–397. PMID: 19064976.
Article10. Deltombe T, Jamart J, Recloux S, Legrand C, Vandenbroeck N, Theys S, et al. Reliability and limits of agreement of circumferential, water displacement, and optoelectronic volumetry in the measurement of upper limb lymphedema. Lymphology. 2007; 40:26–34. PMID: 17539462.11. Szuba A, Shin WS, Strauss HW, Rockson S. The third circulation: radionuclide lymphoscintigraphy in the evaluation of lymphedema. J Nucl Med. 2003; 44:43–57. PMID: 12515876.12. Yuan Z, Chen L, Luo Q, Zhu J, Lu H, Zhu R. The role of radionuclide lymphoscintigraphy in extremity lymphedema. Ann Nucl Med. 2006; 20:341–344. PMID: 16878705.
Article13. Sadeghi R, Kazemzadeh G, Keshtgar M. Diagnostic application of lymphoscintigraphy in the management of lymphoedema. Hell J Nucl Med. 2010; 13:6–10. PMID: 20411162.14. International Society of Lymphology. The diagnosis and treatment of peripheral lymphedema: Consensus document of the International Society of Lymphology. Lymphology. 2003; 36:84–91. PMID: 12926833.15. Dalia RM, Martins GR, Barbosa R, de Lima CF, Siqueira CF. Qualitative and quantitative lymphoscintigraphy in the evaluation of lower limbs lymphedema. Braz Arch Biol Technol. 2005; 48:159–162.
Article16. Hwang JH, Choi JY, Lee JY, Hyun SH, Choi Y, Choe YS, et al. Lymphscintigraphy predicts response to complex physical therapy in patients with early stage extremity lymphedema. Lymphology. 2007; 40:172–176. PMID: 18365531.17. Yoo J, Choi JY, Hwang JH, Kim DI, Kim YW, Choe YS, et al. Prognostic value of lymphoscintigraphy in patients with gynecological cancer-related lymphedema. J Surg Oncol. 2014; 109:760–763. PMID: 24609802.
Article18. Stanton AW, Modi S, Mellor RH, Peters AM, Svensson WE, Levick JR, et al. A quantitative lymphoscintigraphic evaluation of lymphatic function in the swollen hands of women with lymphoedema following breast cancer treatment. Clin Sci (Lond). 2006; 110:553–561. PMID: 16343054.
Article19. Pecking AP, Alberini JL, Wartski M, Edeline V, Cluzan RV. Relationship between lymphoscintigraphy and clinical findings in lower limb lymphedema (LO): toward a comprehensive staging. Lymphology. 2008; 41:1–10. PMID: 18581953.20. Francois A, Richaud C, Bouchet JY, Franco A, Comet M. Does medical treatment of lymphedema act by increasing lymph flow? Vasa. 1989; 18:281–286. PMID: 2609733.21. Franco A, Comet M, Beani JC, Doucet J, Meaulle PY, Guidicelli H. La lymphoscintigraphie indirecte: son intérêt pour le diagnostic étiologique des oedèmes des membres inférieurs de cause non générale. J Biophys Med Nucl. 1980; 4:299–303.22. Szuba A, Strauss W, Sirsikar SP, Rockson SG. Quantitative radionuclide lymphoscintigraphy predicts outcome of manual lymphatic therapy in breast cancer-related lymphedema of the upper extremity. Nucl Med Commun. 2002; 23:1171–1175. PMID: 12464781.
Article23. Kiel KD, Rademacker AW. Early-stage breast cancer: arm edema after wide excision and breast irradiation. Radiology. 1996; 198:279–283. PMID: 8539394.
Article24. Keramopoulos A, Tsionou C, Minaretzis D, Michalas S, Aravantinos D. Arm morbidity following treatment of breast cancer with total axillary dissection: a multivariated approach. Oncology. 1993; 50:445–449. PMID: 8233285.
Article25. Piller N, Carati C. The diagnosis and treatment of peripheral lymphedema. Lymphology. 2009; 42:146–147. PMID: 19938271.26. Shaitelman SF, Cromwell KD, Rasmussen JC, Stout NL, Armer JM, Lasinski BB, et al. Recent progress in the treatment and prevention of cancer-related lymphedema. CA Cancer J Clin. 2015; 65:55–81. PMID: 25410402.
Article27. Cheville AL, McGarvey CL, Petrek JA, Russo SA, Thiadens SR, Taylor ME. The grading of lymphedema in oncology clinical trials. Semin Radiat Oncol. 2003; 13:214–225. PMID: 12903011.
Article28. Armer JM. The problem of post-breast cancer lymphedema: impact and measurement issues. Cancer Invest. 2005; 23:76–83. PMID: 15779870.
Article29. Gebruers N, Truijen S, Engelborghs S, De Deyn PP. Volumetric evaluation of upper extremities in 250 healthy persons. Clin Physiol Funct Imaging. 2007; 27:17–22. PMID: 17204033.
Article30. Smoot BJ, Wong JF, Dodd MJ. Comparison of diagnostic accuracy of clinical measures of breast cancer-related lymphedema: area under the curve. Arch Phys Med Rehabil. 2011; 92:603–610. PMID: 21440706.
Article31. Pain SJ, Barber RW, Ballinger JR, Solanki CK, O'Mahony S, Mortimer PS, et al. Side-to-side symmetry of radioprotein transfer from tissue space to systemic vasculature following subcutaneous injection in normal subjects and patients with breast cancer. Eur J Nucl Med Mol Imaging. 2003; 30:657–661. PMID: 12652333.
Article32. Bar Ad V, Dutta PR, Solin LJ, Hwang WT, Tan KS, Both S, Cheville A, Harris EE. Time-course of arm lymphedema and potential risk factors for progression of lymphedema after breast conservation treatment for early stage breast cancer. Breast J. 2012; 18:219–225. PMID: 22487094.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Quantitative Lymphoscintigraphy to Predict the Possibility of Lymphedema Development After Breast Cancer Surgery: Retrospective Clinical Study
- Acute Traumatic Lymphedema without Tissue Injury Detected by Lymphoscintigraphy
- A Case of Conjunctival and Lid Lymphedema Confirmed with Lymphoscintigraphy
- Early Stage Lymphedema in Breast Cancer Patient Detected by Indocyanine Green Lymphography but not by Lymphoscintigraphy: A Case Report
- Rapid Lymphedema Progression in Breast Cancer Patient with Previous Forearm Fracture