J Korean Soc Radiol.
2016 May;74(5):279-290. 10.3348/jksr.2016.74.5.279.
Interpretation of Neonatal Chest Radiography
- Affiliations
-
- 1Department of Radiology, Kangwon National University Hospital, Chuncheon, Korea. hk2005.yoon@gmail.com
- KMID: 2164823
- DOI: http://doi.org/10.3348/jksr.2016.74.5.279
Abstract
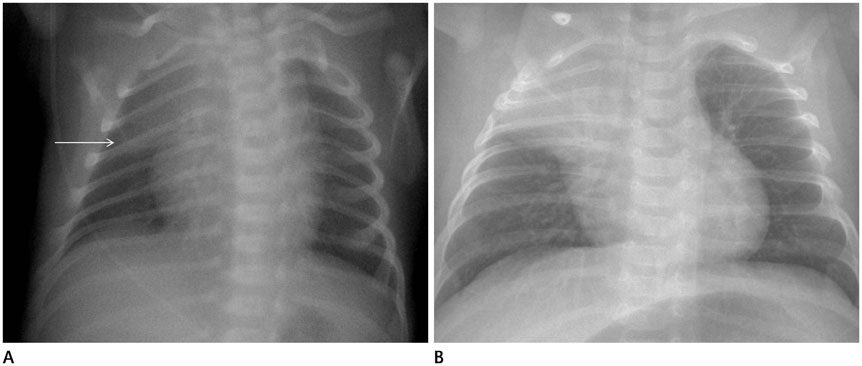
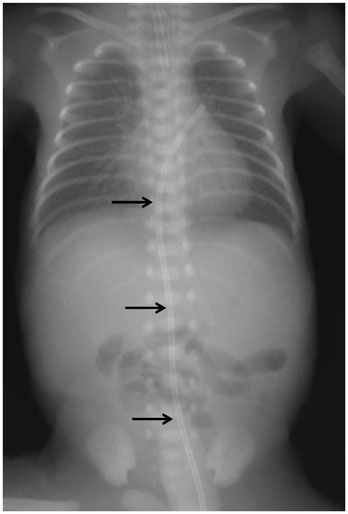
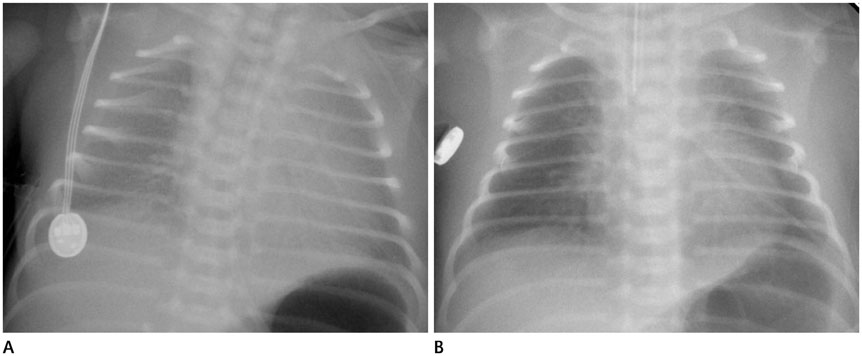
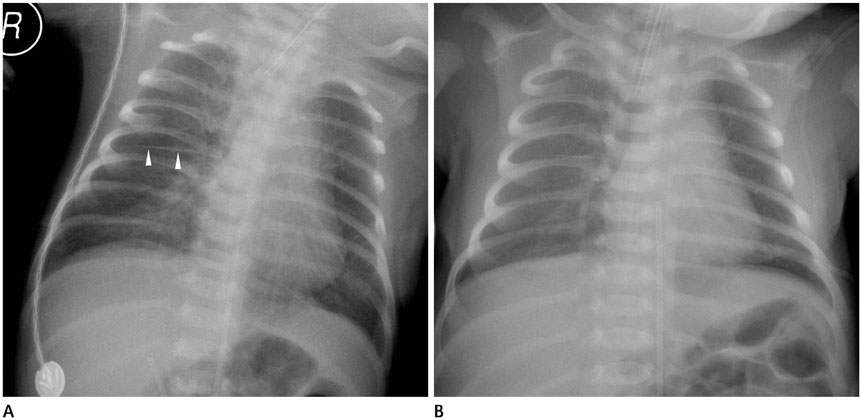
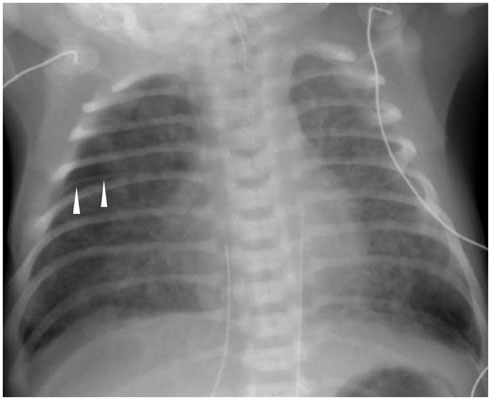
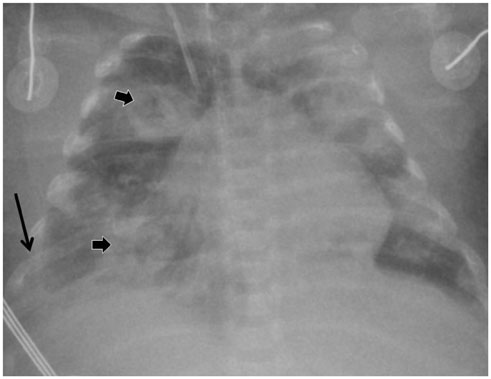
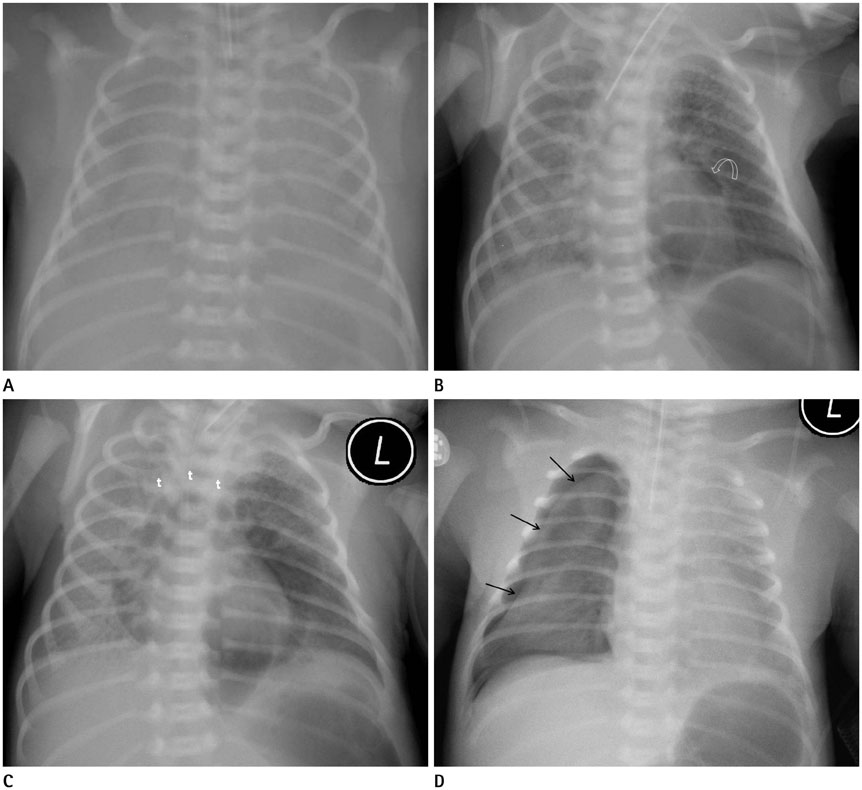
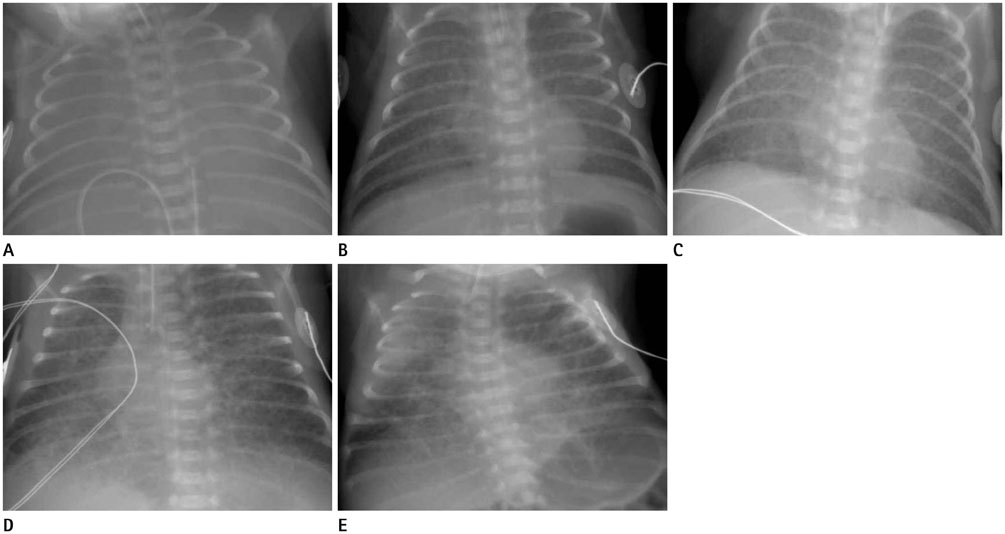
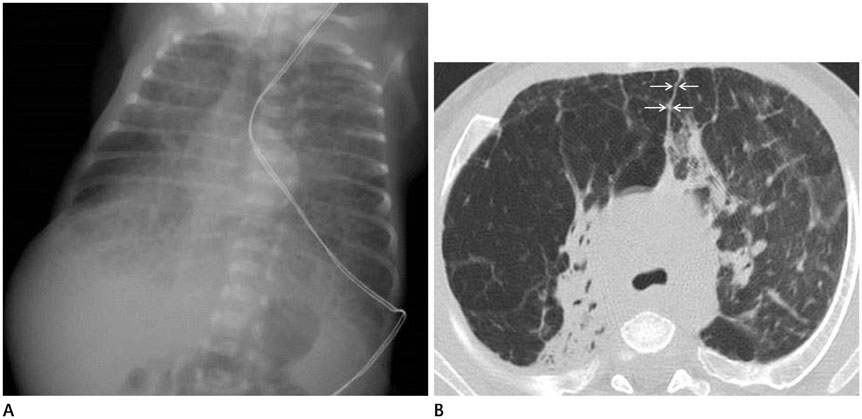
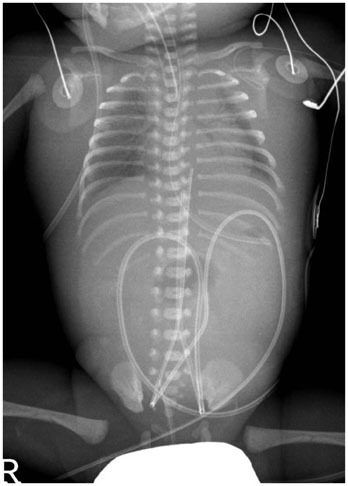
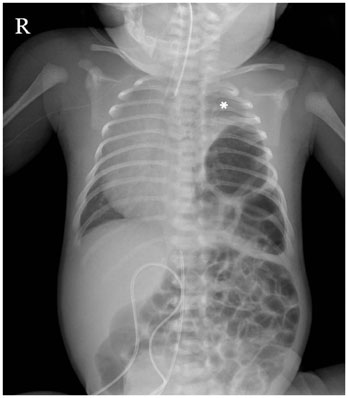
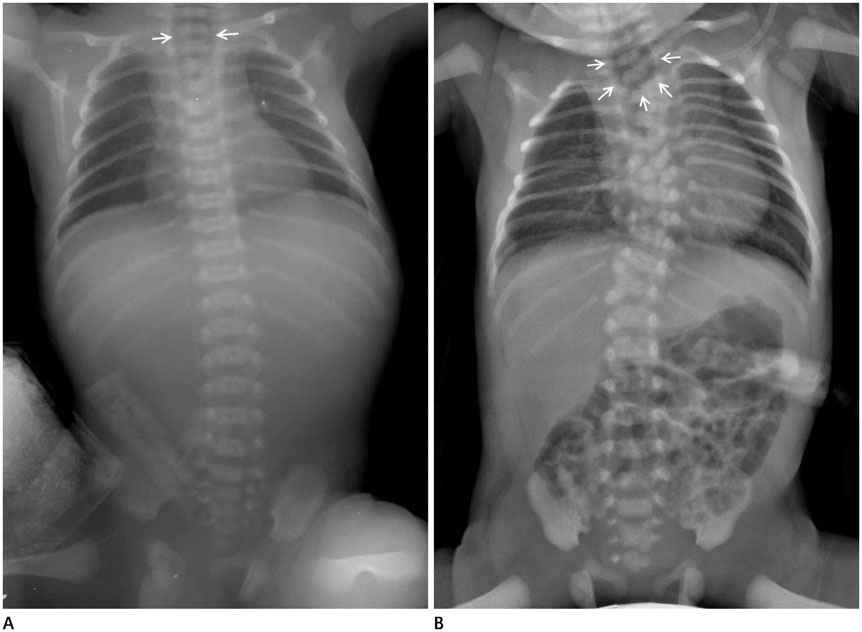
- Plain radiographs for infants in the neonatal intensive care unit are obtained using the portable X-ray equipment in order to evaluate the neonatal lungs and also to check the position of the tubes and catheters used for monitoring critically-ill neonates. Neonatal respiratory distress is caused by a variety of medical or surgical disease conditions. Clinical information about the gestational week, respiratory symptoms, and any events during delivery is essential for interpretation of the neonatal chest radiographs. Awareness of common chest abnormality in the prematurely born or term babies is also very important for chest evaluation in the newborn. Furthermore, knowledge about complications such as air leaks and bronchopulmonary dysplasia following treatment are required to accurately inform the clinicians. The purpose of this article was to briefly review radiographic findings of chest diseases in newborns that are relatively common in daily practice.
MeSH Terms
Figure
Reference
-
1. Cleveland RH. A radiologic update on medical diseases of the newborn chest. Pediatr Radiol. 1995; 25:631–637.2. Choi YH, Kim IO. Neonatal chest imaging. In : Kim IO, editor. Radiology Illustrated: Pediatric Radiology. Berlin Heidelberg: Springer-Verlag;2014. p. 381–409.3. Kim JH, Lee YS, Kim SH, Lee SK, Lim MK, Kim HS. Does umbilical vein catheterization lead to portal venous thrombosis? Prospective US evaluation in 100 neonates. Radiology. 2001; 219:645–650.4. Agrons GA, Courtney SE, Stocker JT, Markowitz RI. From the archives of the AFIP: lung disease in premature neonates: radiologic-pathologic correlation. Radiographics. 2005; 25:1047–1073.5. Slama M, André C, Huon C, Antoun H, Adamsbaum C. Radiological analysis of hyaline membrane disease after exogenous surfactant treatment. Pediatr Radiol. 1999; 29:56–60.6. Ross MG. Meconium aspiration syndrome--more than intrapartum meconium. N Engl J Med. 2005; 353:946–948.7. Nissen MD. Congenital and neonatal pneumonia. Paediatr Respir Rev. 2007; 8:195–203.8. Bowen A 3rd, Quattromani FL. Infraazygous pneumomediastinum in the newborn. AJR Am J Roentgenol. 1980; 135:1017–1021.9. Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001; 163:1723–1729.10. Howling SJ, Northway WH Jr, Hansell DM, Moss RB, Ward S, Müller NL. Pulmonary sequelae of bronchopulmonary dysplasia survivors: high-resolution CT findings. AJR Am J Roentgenol. 2000; 174:1323–1326.11. Shih YT, Su PH, Chen JY, Lee IC, Hu JM, Chang HP. Common etiologies of neonatal pleural effusion. Pediatr Neonatol. 2011; 52:251–255.12. Irish MS, Holm BA, Glick PL. Congenital diaphragmatic hernia. A historical review. Clin Perinatol. 1996; 23:625–653.