J Korean Soc Radiol.
2016 Jun;74(6):412-416. 10.3348/jksr.2016.74.6.412.
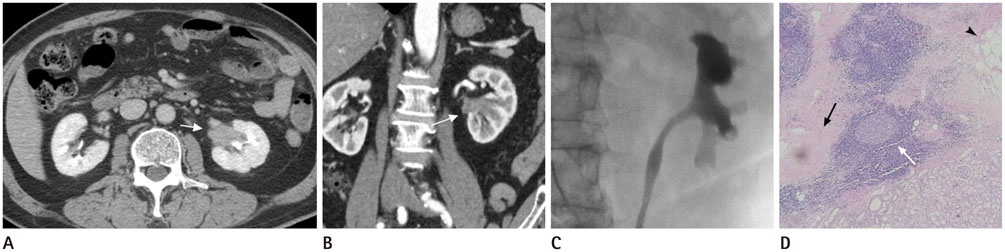
Idiopathic Retroperitoneal Fibrosis Involving a Unilateral Renal Sinus: A Case Report and Literature Review
- Affiliations
-
- 1Department of Radiology, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea. radyjh@hanmail.net
- KMID: 2164821
- DOI: http://doi.org/10.3348/jksr.2016.74.6.412
Abstract
- Idiopathic retroperitoneal fibrosis (RPF) is a rare disease entity and its etiology is uncertain. We report two similar cases which showed an uncommon presentation of idiopathic RPF. A 66-year-old woman and an 80-year-old man presented with incidental findings of left renal pelvic mass-like lesions. Computed tomography revealed a soft tissue density mass replacing the left renal pelvis, which was suspicious for renal pelvic cancer, and the diagnosis of idiopathic RPF was surgically confirmed. To the best of our knowledge, a few cases of idiopathic RPF presenting with features of a localized unilateral renal pelvic mass mimicking renal pelvic cancer have been reported.
MeSH Terms
Figure
Reference
-
1. Vaglio A, Salvarani C, Buzio C. Retroperitoneal fibrosis. Lancet. 2006; 367:241–251.2. Amis ES Jr. Retroperitoneal fibrosis. AJR Am J Roentgenol. 1991; 157:321–329.3. Vaglio A, Buzio C. Chronic periaortitis: a spectrum of diseases. Curr Opin Rheumatol. 2005; 17:34–40.4. Kottra JJ, Dunnick NR. Retroperitoneal fibrosis. Radiol Clin North Am. 1996; 34:1259–1275.5. Warakaulle DR, Prematilleke I, Moore NR. Retroperitoneal fibrosis mimicking retrocrural lymphadenopathy. Clin Radiol. 2004; 59:292–293.6. Ergen FB, Arslan EB, Turkbey B, Akinci D, Akata D. Unilateral perirenal fibrosis. J Comput Assist Tomogr. 2005; 29:477–480.7. Ayuso JR, Garcia-Criado A, Caralt TM, Ayuso C, Torras A, Ribalta T. Atypical retroperitoneal fibrosis: MRI findings. Eur Radiol. 1999; 9:937–939.8. Yoshino T, Moriyama H, Fukushima M, Sanda N. A case of IgG4-related retroperitoneal fibrosis mimicking renal pelvic cancer. Urol Int. 2013; 90:365–368.9. Lang JT, Kang N, Zhang JH, Xing NZ. Unilateral perirenal fibrosis without aorta involvement. Eur Rev Med Pharmacol Sci. 2015; 19:732–735.10. Seo N, Kim JH, Byun JH, Lee SS, Kim HJ, Lee MG. Immunoglobulin G4-related kidney disease: a comprehensive pictorial review of the imaging spectrum, mimickers, and clinicopathological characteristics. Korean J Radiol. 2015; 16:1056–1067.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Idiopathic Retroperitoneal Fibrosis: Report of a Case
- A Case of Idiopathic Retroperitoneal Fibrosis Treated by Bilateral Pyeloileoneocystostomy
- A Case of Idiopathic Retroperitoneal Fibrosis with Acute Renal Failure and a Pleural Effusion
- A case of idiopathic retroperitoneal fibrosis with chronic renal failure undergoing maintenance hemodialysis
- Idiopathic Retroperitoneal Fibrosis Treated with High Dose Steroids