Yonsei Med J.
2015 Sep;56(5):1453-1456. 10.3349/ymj.2015.56.5.1453.
Invasive Primary Colonic Aspergillosis in the Immunocompetent Host without Classical Risk Factors
- Affiliations
-
- 1Department of Internal Medicine, School of Medicine, The Catholic University of Korea, St. Vincent's Hospital, Suwon, Korea. cttailor@catholic.ac.kr
- KMID: 2163644
- DOI: http://doi.org/10.3349/ymj.2015.56.5.1453
Abstract
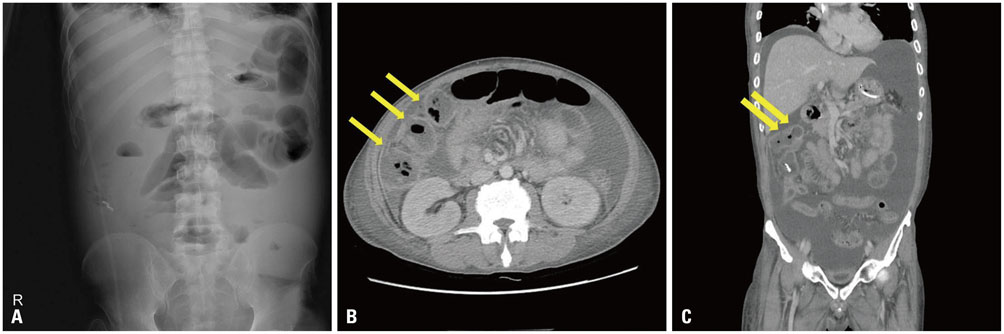
- Invasive aspergillosis (IA), generally considered an opportunistic infection in immunocompromised hosts, is associated with high morbidity and mortality. IA commonly occurs in the respiratory tract with isolated reports of aspergillosis infection in the nasal sinuses, central nervous system, skin, liver, and urinary tract. Extra-pulmonary aspergillosis is usually observed in disseminated disease. To date, there are a few studies regarding primary and disseminated gastrointestinal (GI) aspergillosis in immunocompromised hosts. Only a few cases of primary GI aspergillosis in non-immunocompromised hosts have been reported; of these, almost all of them involved the upper GI tract. We describe a very rare case of IA involving the lower GI tract in the patient without classical risk factors that presented as multiple colon perforations and was successfully treated by surgery and antifungal treatment. We also review related literature and discuss the characteristics and risk factors of IA in the immunocompetent hosts without classical risk factors. This case that shows IA should be considered in critically ill patients, and that primary lower GI aspergillosis may also occur in the immunocompetent hosts without classical risk factors.
MeSH Terms
-
Amphotericin B/administration & dosage/therapeutic use
Antifungal Agents/administration & dosage/*therapeutic use
Aspergillosis/*diagnosis/drug therapy/microbiology/surgery
Aspergillus/*isolation & purification
Colon/microbiology/radiography/*surgery
Colonic Diseases/diagnosis/therapy
Combined Modality Therapy
Humans
*Immunocompetence
Laparotomy
Male
Middle Aged
Treatment Outcome
Voriconazole/administration & dosage/therapeutic use
Amphotericin B
Antifungal Agents
Voriconazole
Figure
Cited by 2 articles
-
Methidathion Poisoning
Ki Hoon Kim, Se Hun Kim, Charles Her
Korean J Crit Care Med. 2017;32(4):363-369. doi: 10.4266/kjccm.2016.00073.Primary Invasive Intestinal Aspergillosis in a Non-Severely Immunocompromised Patient
Eunmi Gil, Tae Sun Ha, Gee Young Suh, Chi Ryang Chung, Chi-Min Park
Korean J Crit Care Med. 2016;31(2):129-133. doi: 10.4266/kjccm.2016.31.2.129.
Reference
-
1. Segal BH. Aspergillosis. N Engl J Med. 2009; 360:1870–1884.2. Maertens J, Vrebos M, Boogaerts M. Assessing risk factors for systemic fungal infections. Eur J Cancer Care (Engl). 2001; 10:56–62.3. Stevens DA, Melikian GL. Aspergillosis in the 'nonimmunocompromised' host. Immunol Invest. 2011; 40:751–766.
Article4. Eggimann P, Chevrolet JC, Starobinski M, Majno P, Totsch M, Chapuis B, et al. Primary invasive aspergillosis of the digestive tract: report of two cases and review of the literature. Infection. 2006; 34:333–338.
Article5. Kazan E, Maertens J, Herbrecht R, Weisser M, Gachot B, Vekhoff A, et al. A retrospective series of gut aspergillosis in haematology patients. Clin Microbiol Infect. 2011; 17:588–594.
Article6. Meersseman W, Lagrou K, Maertens J, Van Wijngaerden E. Invasive aspergillosis in the intensive care unit. Clin Infect Dis. 2007; 45:205–216.7. Kox WJ, Volk T, Kox SN, Volk HD. Immunomodulatory therapies in sepsis. Intensive Care Med. 2000; 26:Suppl 1. S124–S128.8. Delamaire M, Maugendre D, Moreno M, Le Goff MC, Allannic H, Genetet B. Impaired leucocyte functions in diabetic patients. Diabet Med. 1997; 14:29–34.
Article9. Hostetter MK. Handicaps to host defense. Effects of hyperglycemia on C3 and Candida albicans. Diabetes. 1990; 39:271–275.
Article10. Graham PL 3rd, Lin SX, Larson EL. A U.S. population-based survey of Staphylococcus aureus colonization. Ann Intern Med. 2006; 144:318–325.
Article11. Choi SH, Chung JW, Cho SY, Kim BJ, Kwon GY. A case of isolated invasive Aspergillus colitis presenting with hematochezia in a nonneutropenic patient with colon cancer. Gut Liver. 2010; 4:274–277.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Invasive Pulmonary Aspergillosis Invaded to Thoracic Vertebra in a Immunocompetent Host: A case report
- Cutaneous Aspergillosis
- Acute Respiratory Failure from Invasive Pulmonary Aspergillosis in an Immunocompetent Adult: A Case Report
- A Case of Invasive Pulmonary Aspergillosis in an Jmmunocompetent Host
- A Case of Primary Cutaneous Aspergillosis on the Scalp and the Neck