Investig Magn Reson Imaging.
2016 Mar;20(1):9-26. 10.13104/imri.2016.20.1.9.
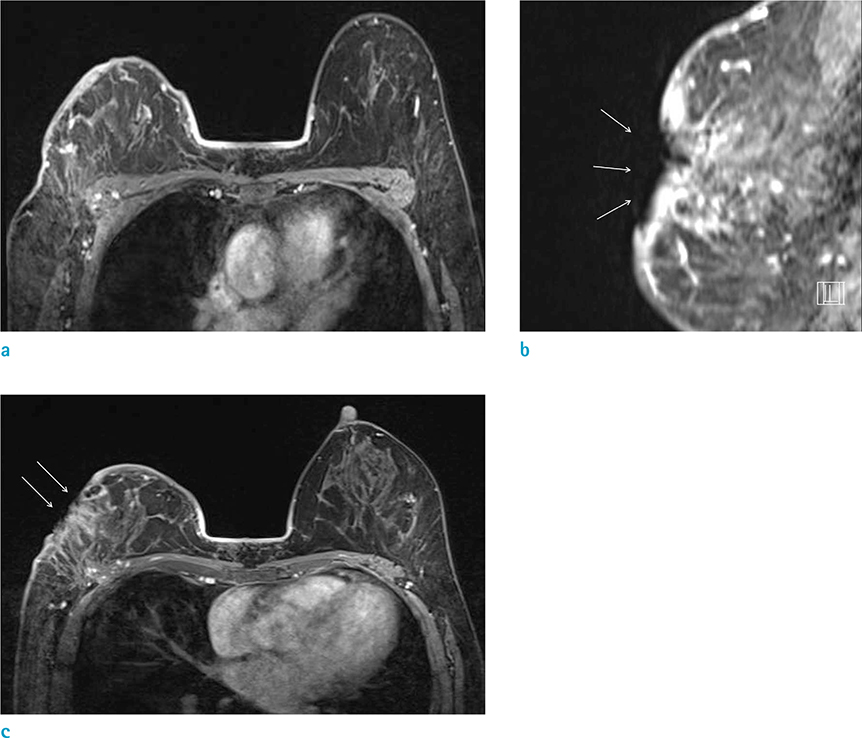
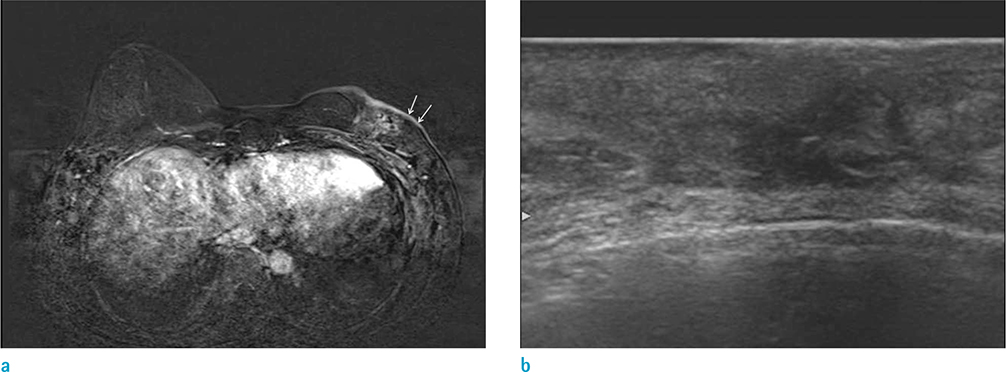
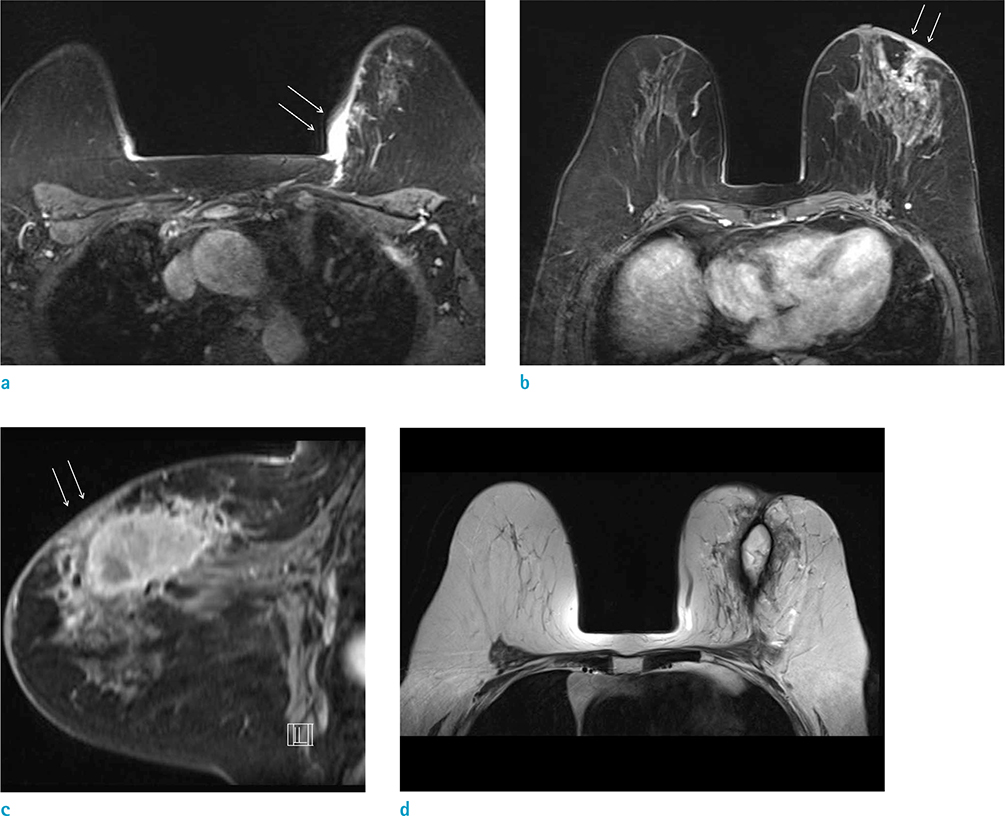
Imaging and Pathologic Characterization of the Skin Thickening or Enhancement under the Breast MRI
- Affiliations
-
- 1Department of Radiology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. lionmain@catholic.ac.kr
- KMID: 2161366
- DOI: http://doi.org/10.13104/imri.2016.20.1.9
Abstract
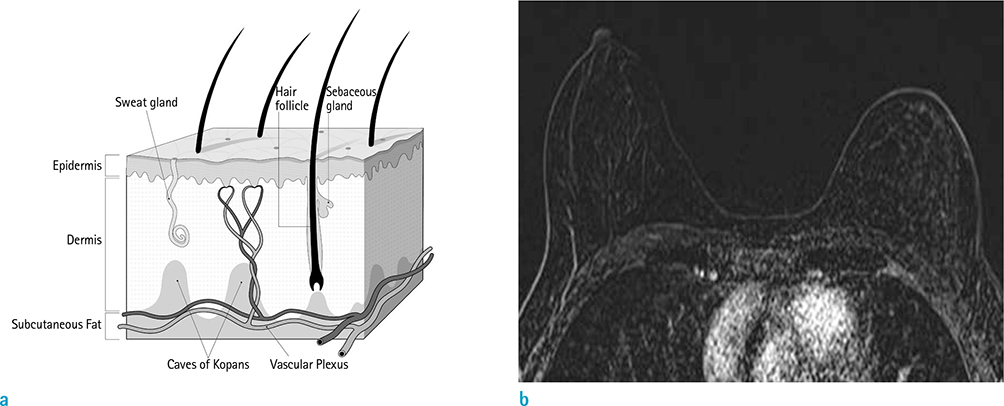
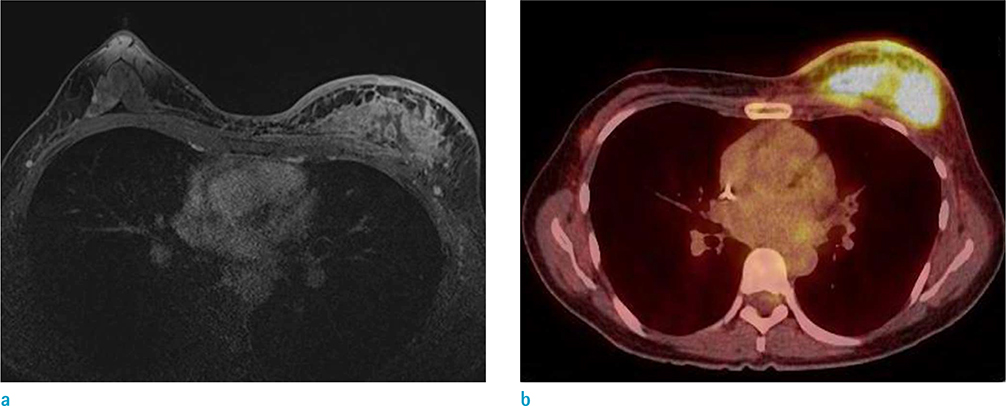
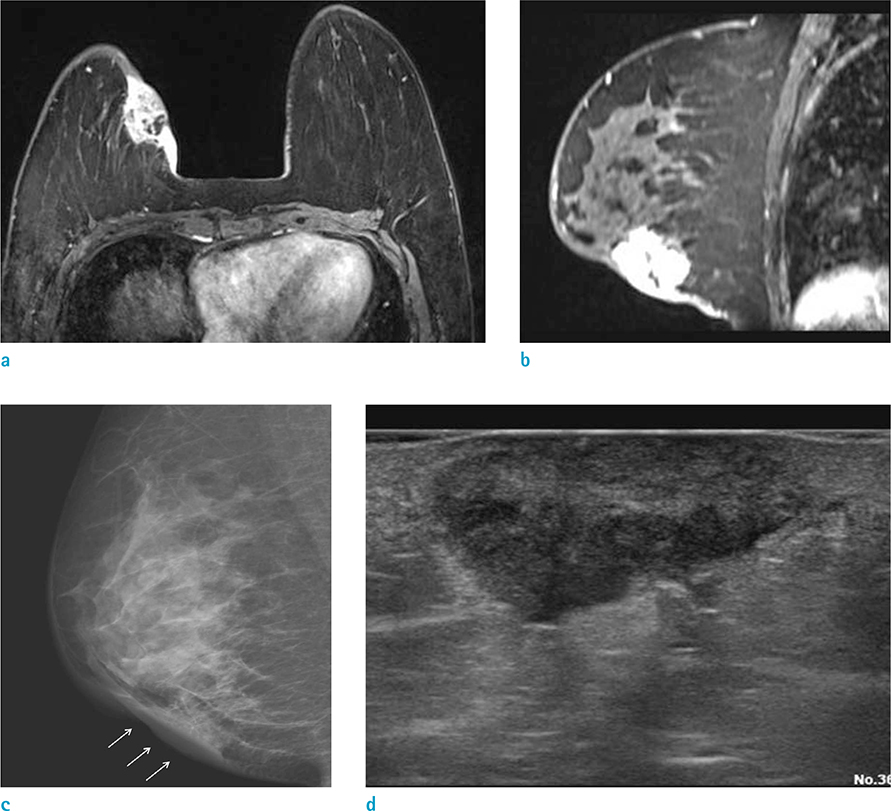
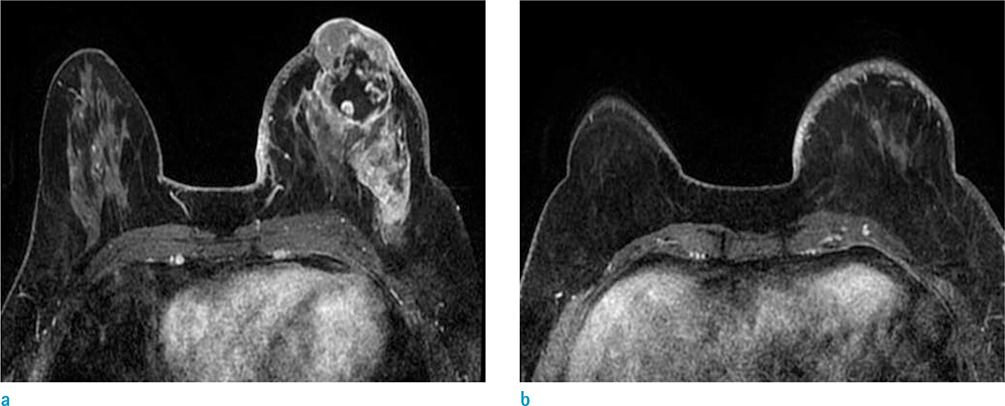
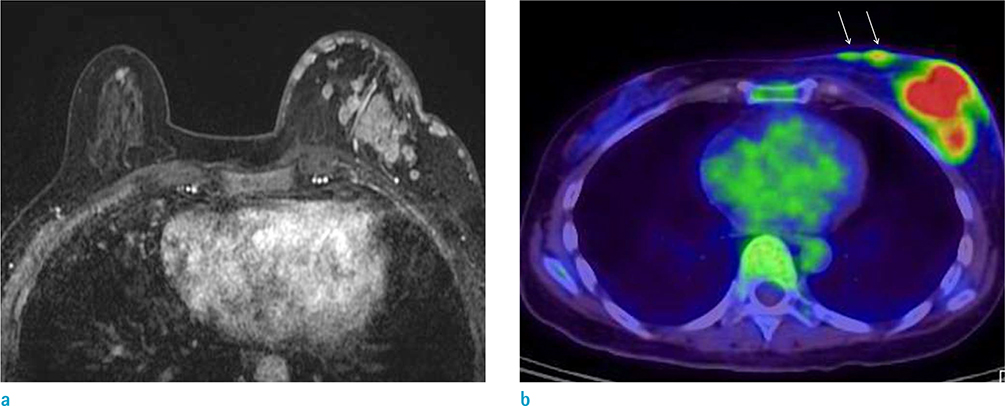
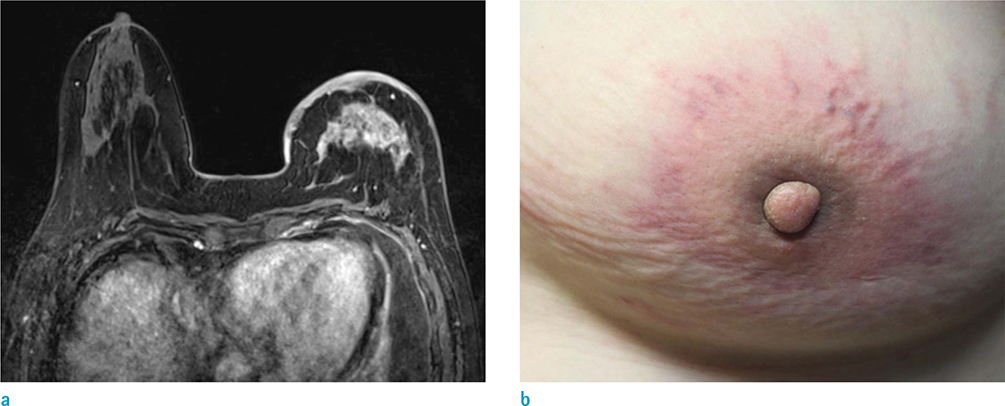
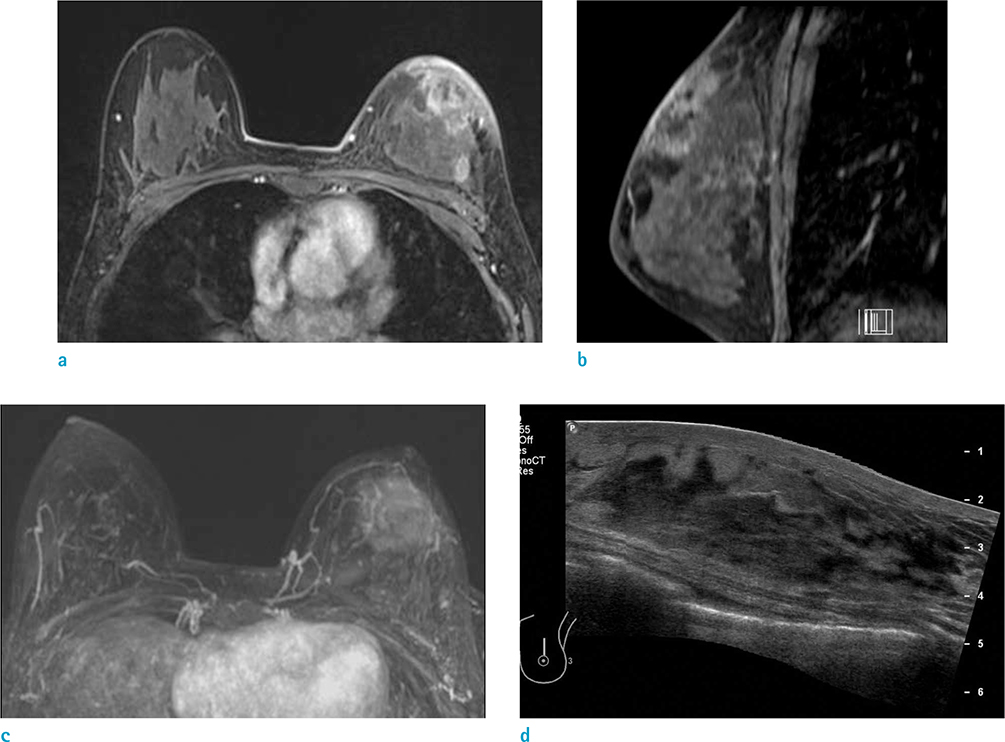
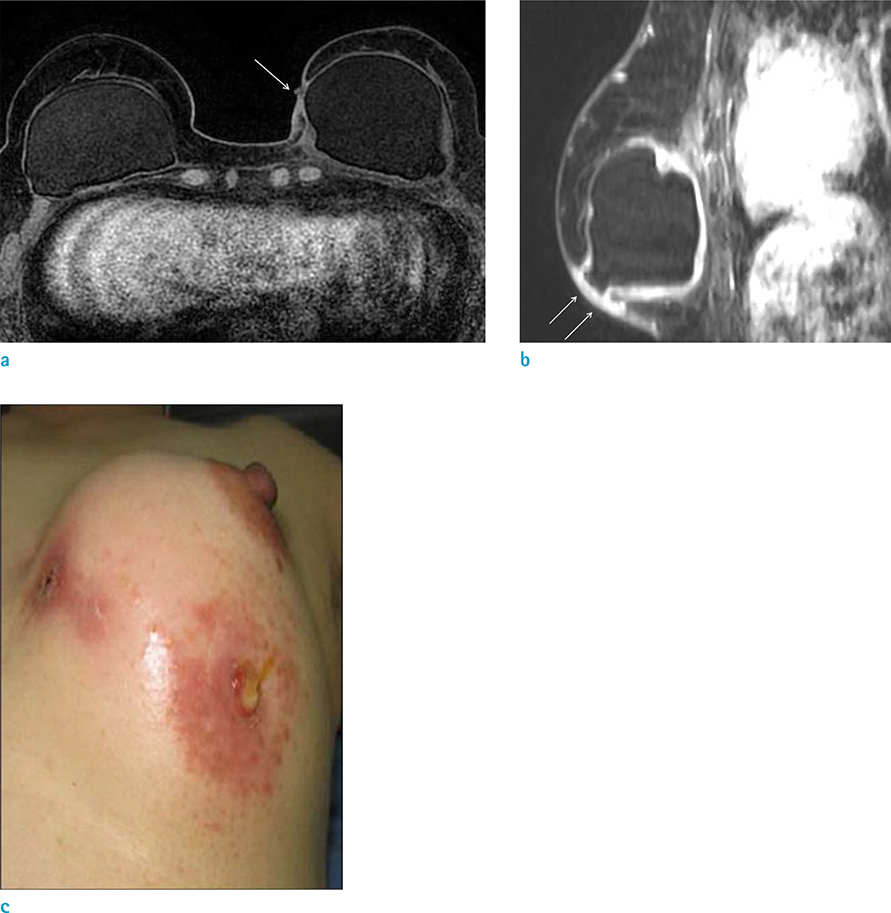
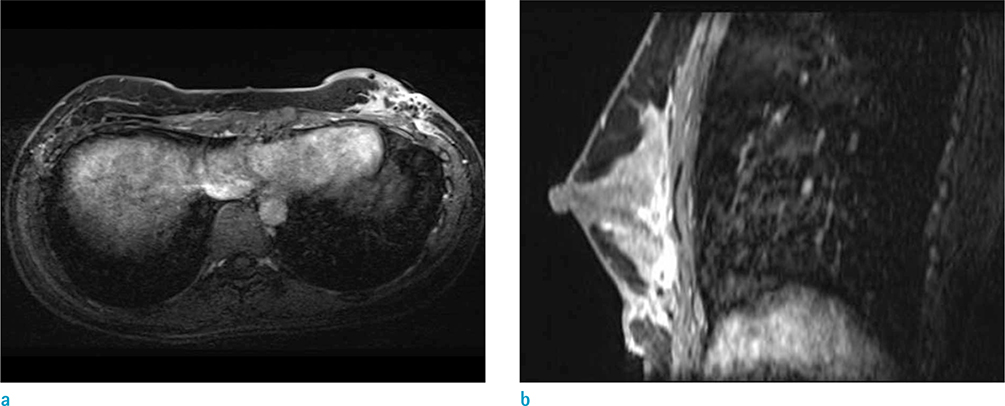
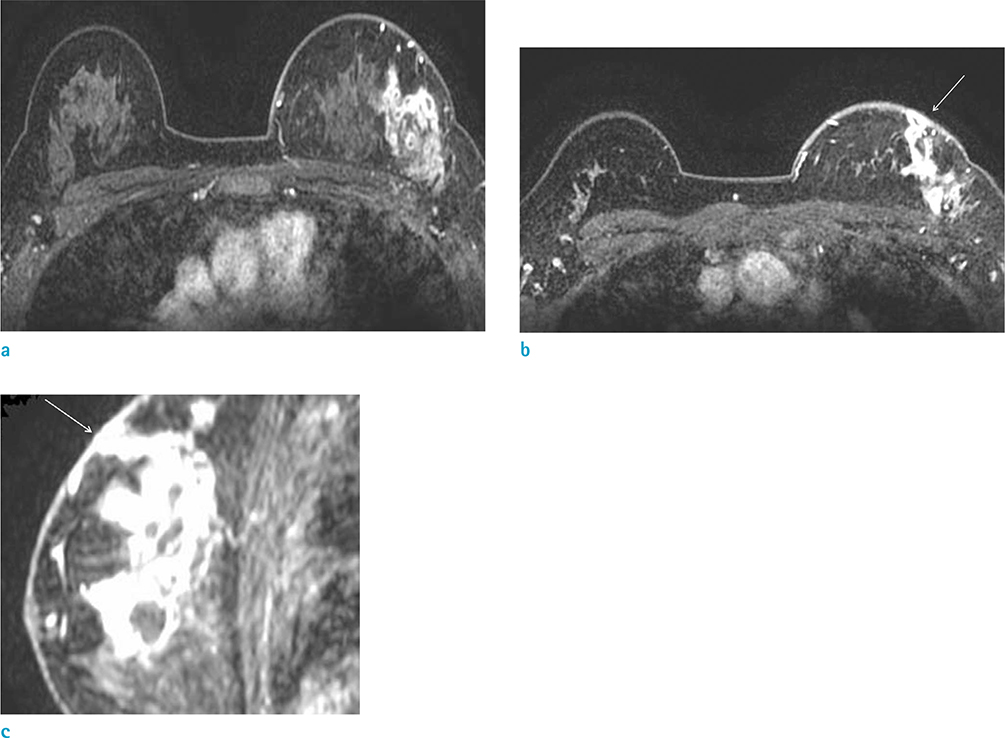
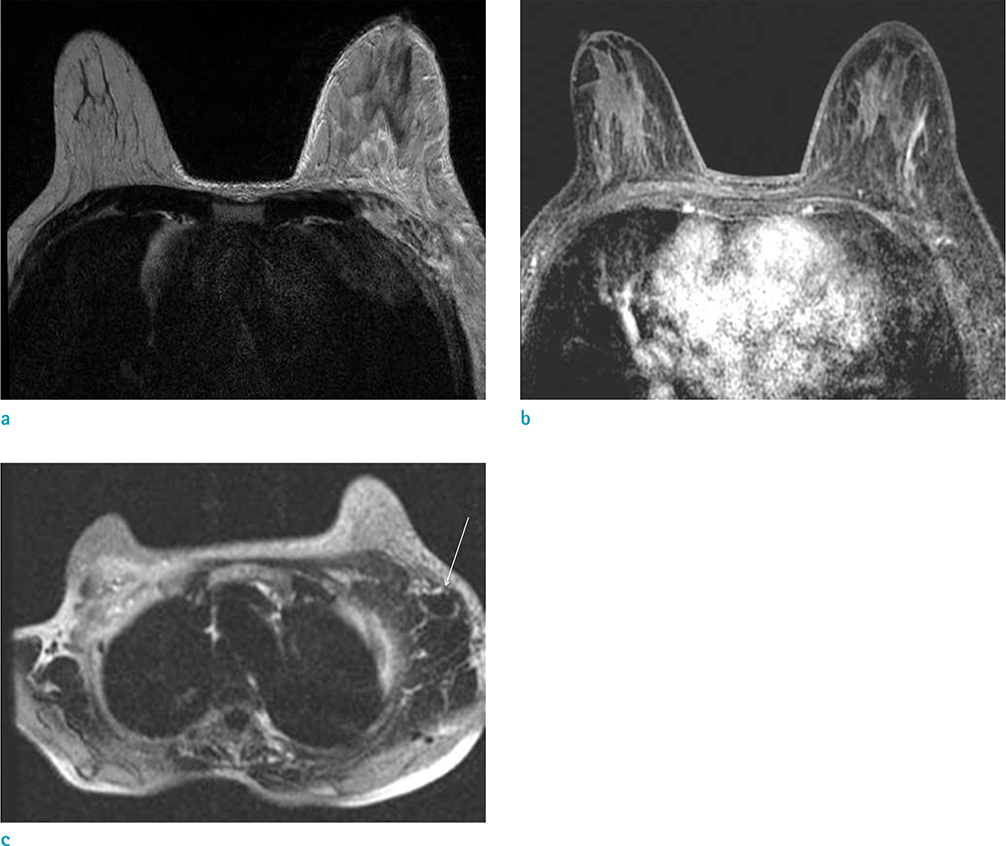
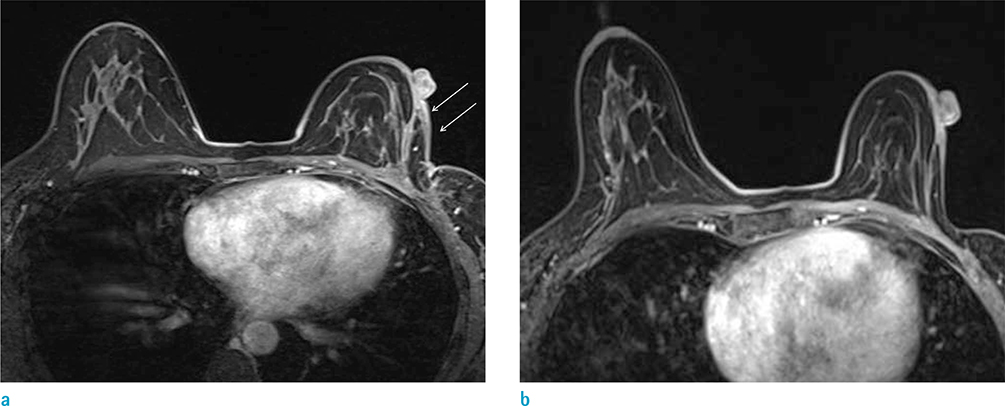
- The purpose of this paper is to show the radiologic features of various lesions appearing as skin thickening or enhancement under the breast MRI. And histopathologic results of the skin lesions were correlated. Radiologist must be familiar with normal appearance of the breast skin under the MRI and a wide variety of conditions may affect the skin of the breast.
Keyword
Figure
Cited by 1 articles
-
Introduction of a New Staging System of Breast Cancer for Radiologists: An Emphasis on the Prognostic Stage
Jieun Koh, Min Jung Kim
Korean J Radiol. 2019;20(1):69-82. doi: 10.3348/kjr.2018.0231.
Reference
-
1. Kalli S, Freer PE, Rafferty EA. Lesions of the skin and superficial tissue at breast MR imaging. Radiographics. 2010; 30:1891–1913.2. Morris EA, Liberman L. Breast MRI: diagnosis and intervention. 2005; New York, NY: Springer.3. Dershaw DD, Moore MP, Liberman L, Deutch BM. Inflammatory breast carcinoma: mammographic findings. Radiology. 1994; 190:831–834.4. Ellis DL, Teitelbaum SL. Inflammatory carcinoma of the breast. A pathologic definition. Cancer. 1974; 33:1045–1047.5. Yang WT, Le-Petross HT, Macapinlac H, et al. Inflammatory breast cancer: PET/CT, MRI, mammography, and sonography findings. Breast Cancer Res Treat. 2008; 109:417–426.6. Le-Petross HT, Cristofanilli M, Carkaci S, et al. MRI features of inflammatory breast cancer. AJR Am J Roentgenol. 2011; 197:W769–W776.7. Le-Petross CH, Bidaut L, Yang WT. Evolving role of imaging modalities in inflammatory breast cancer. Semin Oncol. 2008; 35:51–63.8. Girardi V, Carbognin G, Camera L, et al. Inflammatory breast carcinoma and locally advanced breast carcinoma: characterisation with MR imaging. Radiol Med. 2011; 116:71–83.9. Anderson WF, Chu KC, Chang S. Inflammatory breast carcinoma and noninflammatory locally advanced breast carcinoma: distinct clinicopathologic entities? J Clin Oncol. 2003; 21:2254–2259.10. Renz DM, Baltzer PA, Bottcher J, et al. Inflammatory breast carcinoma in magnetic resonance imaging: a comparison with locally advanced breast cancer. Acad Radiol. 2008; 15:209–221.11. Haagensen CD, Stout AP. Carcinoma of the breast. II-Criteria of operability. Ann Surg. 1943; 859–870.12. Haagensen CD, Bodian C. A personal experience with Halsted's radical mastectomy. Ann Surg. 1984; 199:143–150.13. Gueth U, Wight E, Schoetzau A, et al. Non-inflammatory skin involvement in breast cancer, histologically proven but without the clinical and histological T4 category features. J Surg Oncol. 2007; 95:291–297.14. Guth U, Singer G, Langer I, et al. T4 category revision enhances the accuracy and significance of stage III breast cancer. Cancer. 2006; 106:2569–2575.15. Guth U, Wight E, Schotzau A, et al. A new approach in breast cancer with non-inflammatory skin involvement. Acta Oncol. 2006; 45:576–583.16. Guth U, Wight E, Singer G. Breast cancer with noninflammatory skin involvement: new data revise the traditional image of a "classical" clinicopathologic entity. Praxis (Bern 1994). 2006; 95:1829–1835.17. Wieland AW, Louwman MW, Voogd AC, van Beek MW, Vreugdenhil G, Roumen RM. Determinants of prognosis in breast cancer patients with tumor involvement of the skin (pT4b). Breast J. 2004; 10:123–128.18. Stavros AT, Rapp CL, Parker SH. Breast ultrasound. 2004; Philadelphia: Lippincott Williams & Wilkins.19. Kamby C, Andersen J, Ejlertsen B, et al. Pattern of spread and progression in relation to the characteristics of the primary tumour in human breast cancer. Acta Oncol. 1991; 30:301–308.20. Orel SG, Fowble BL, Solin LJ, Schultz DJ, Conant EF, Troupin RH. Breast cancer recurrence after lumpectomy and radiation therapy for early-stage disease: prognostic significance of detection method. Radiology. 1993; 188:189–194.21. Ralleigh G, Walker AE, Hall-Craggs MA, Lakhani SR, Saunders C. MR imaging of the skin and nipple of the breast: differentiation between tumour recurrence and post-treatment change. Eur Radiol. 2001; 11:1651–1658.22. Voogd AC, van Tienhoven G, Peterse HL, et al. Local recurrence after breast conservation therapy for early stage breast carcinoma: detection, treatment, and outcome in 266 patients. Dutch Study Group on Local Recurrence after Breast Conservation (BORST). Cancer. 1999; 85:437–446.23. Vaughan A, Dietz JR, Aft R, et al. Scientific Presentation Award. Patterns of local breast cancer recurrence after skin-sparing mastectomy and immediate breast reconstruction. Am J Surg. 2007; 194:438–443.24. Bolin DJ, Lukas GM. Low-grade dermal angiosarcoma of the breast following radiotherapy. Am Surg. 1996; 62:668–672.25. Fineberg S, Rosen PP. Cutaneous angiosarcoma and atypical vascular lesions of the skin and breast after radiation therapy for breast carcinoma. Am J Clin Pathol. 1994; 102:757–763.26. Hunter TB, Martin PC, Dietzen CD, Tyler LT. Angiosarcoma of the breast. Two case reports and a review of the literature. Cancer. 1985; 56:2099–2106.27. Sanders LM, Groves AC, Schaefer S. Cutaneous angiosarcoma of the breast on MRI. AJR Am J Roentgenol. 2006; 187:W143–W146.28. Nouri K. Skin cancer. New York: McGraw-Hill Medical;2008.29. Nebesio CL, Goulet RJ, Jr , Helft PR, Billings SD. Metastatic esophageal carcinoma masquerading as inflammatory breast carcinoma. Int J Dermatol. 2007; 46:303–305.30. Sy AN, Lam TP, Khoo US. Subcutaneous panniculitislike T-cell lymphoma appearing as a breast mass: a difficult and challenging case appearing at an unusual site. J Ultrasound Med. 2005; 24:1453–1460.31. Uematsu T, Kasami M. 3T-MRI, elastography, digital mammography, and FDG-PET CT findings of subcutaneous panniculitis-like T-cell lymphoma (SPTCL) of the breast. Jpn J Radiol. 2012; 30:766–771.32. Shim E, Song SE, Seo BK, Kim YS, Son GS. Lymphoma affecting the breast: a pictorial review of multimodal imaging findings. J Breast Cancer. 2013; 16:254–265.33. Crowe DJ, Helvie MA, Wilson TE. Breast infection. Mammographic and sonographic findings with clinical correlation. Invest Radiol. 1995; 30:582–587.34. Ulitzsch D, Nyman MK, Carlson RA. Breast abscess in lactating women: US-guided treatment. Radiology. 2004; 232:904–909.35. Renz DM, Baltzer PA, Bottcher J, et al. Magnetic resonance imaging of inflammatory breast carcinoma and acute mastitis. A comparative study. Eur Radiol. 2008; 18:2370–2380.36. Fletcher A, Magrath IM, Riddell RH, Talbot IC. Granulomatous mastitis: a report of seven cases. J Clin Pathol. 1982; 35:941–945.37. Han BK, Choe YH, Park JM, et al. Granulomatous mastitis: mammographic and sonographic appearances. AJR Am J Roentgenol. 1999; 173:317–320.38. Van Ongeval C, Schraepen T, Van Steen A, Baert AL, Moerman P. Idiopathic granulomatous mastitis. Eur Radiol. 1997; 7:1010–1012.39. Gautier N, Lalonde L, Tran-Thanh D, et al. Chronic granulomatous mastitis: imaging, pathology and management. Eur J Radiol. 2013; 82:e165–e175.40. Kwak JY, Kim EK, Chung SY, et al. Unilateral breast edema: spectrum of etiologies and imaging appearances. Yonsei Med J. 2005; 46:1–7.41. Heywang-Kobrunner SH, Schlegel A, Beck R, et al. Contrast-enhanced MRI of the breast after limited surgery and radiation therapy. J Comput Assist Tomogr. 1993; 17:891–900.42. Wu F, Wang ZB, Chen WZ, et al. Extracorporeal high intensity focused ultrasound ablation in the treatment of 1038 patients with solid carcinomas in China: an overview. Ultrason Sonochem. 2004; 11:149–154.43. Taboada JL, Stephens TW, Krishnamurthy S, Brandt KR, Whitman GJ. The many faces of fat necrosis in the breast. AJR Am J Roentgenol. 2009; 192:815–825.44. Giess CS, Raza S, Birdwell RL. Distinguishing breast skin lesions from superficial breast parenchymal lesions: diagnostic criteria, imaging characteristics, and pitfalls. Radiographics. 2011; 31:1959–1972.45. Iglesias A, Arias M, Santiago P, Rodriguez M, Manas J, Saborido C. Benign breast lesions that simulate malignancy: magnetic resonance imaging with radiologic-pathologic correlation. Curr Probl Diagn Radiol. 2007; 36:66–82.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Benefit of Sonography in Pregnancy-associated Breast Cancer
- Role of MRI in Diagnostic Evaluation of Papillary Lesions of the Breast
- The Role of Preoperative Breast MRI in Patients With Early-Stage Breast Cancer
- Imaging Diagnosis of Breast Tuberculosis
- Diffusion-Weighted Imaging as a Stand-Alone Breast Imaging Modality