Yonsei Med J.
2008 Oct;49(5):757-764. 10.3349/ymj.2008.49.5.757.
Diagnosis of Pseudoangiomatous Stromal Hyperplasia of the Breast: Ultrasonography Findings and Different Biopsy Methods
- Affiliations
-
- 1Department of Radiology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. claudel@skku.edu
- 2Department of Radiology, Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2158194
- DOI: http://doi.org/10.3349/ymj.2008.49.5.757
Abstract
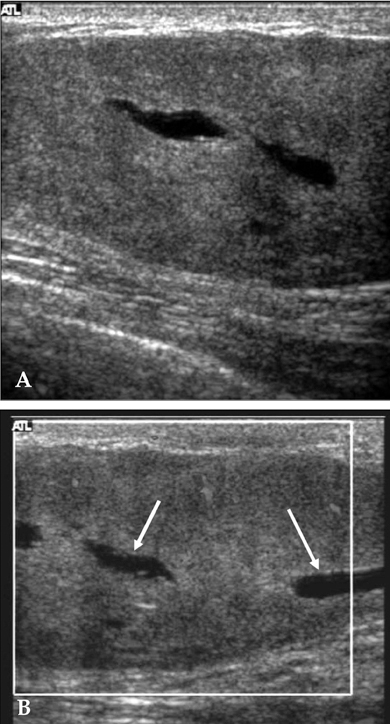
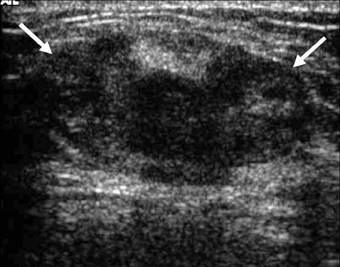
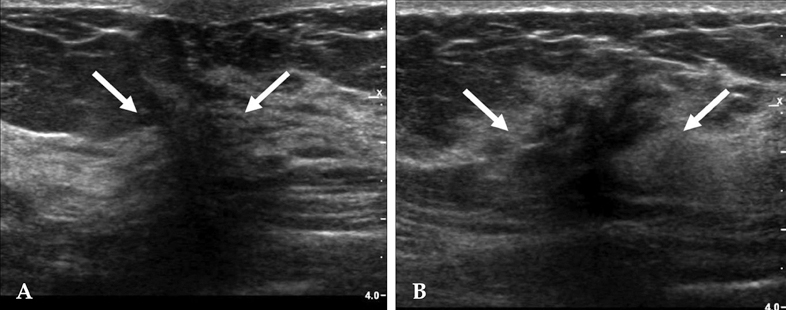
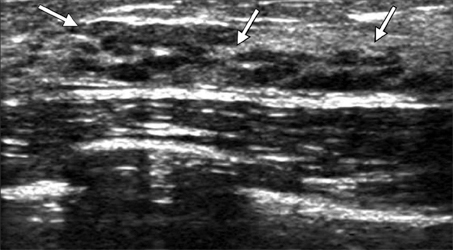
- PURPOSE
Pseudoangiomatous stromal hyperplasia (PASH) of the breast is a rare, benign condition that can be mistaken as a fibroadenoma on an ultrasound examination or as a low-grade angiosarcoma on a histological examination. The objective of this study was to evaluate the ultrasound features and to present biopsy methods to correctly identify PASH. PATIENTS AND METHODS: We retrospectively reviewed the data of 55 women who were diagnosed with PASH of the breast. Ultrasound features were evaluated according to the Breast Imaging Reporting and Data System (BI-RADS; American College of Radiology). The diagnostic ability of different biopsy methods such as core needle biopsy, vacuum-assisted biopsy and excisional biopsy were analyzed with the final histopathological results of surgical specimens. RESULTS: PASH presented as a circumscribed solid mass, with hypoechoic texture with or without heterogeneity, and a parallel orientation. The features of small, internal cysts or vascular channels and no calcifications can be used to differentiate the lesions from fibroadenomas. A core needle biopsy misdiagnosed PASH in 13 cases out of 28 cases and vacuum-assisted biopsy correctly identified PASH in all 3 cases. CONCLUSION: Ultrasound features of PASH should be noted when performing a biopsy. For inconclusive cases of PASH, an excisional biopsy followed by an initial core biopsy should be performed.
MeSH Terms
Figure
Reference
-
1. Vuitch MF, Rosen PP, Erlandson RA. Pseudoangiomatous hyperplasia of mammary stroma. Hum Pathol. 1986. 17:185–191.
Article2. Cohen MA, Morris EA, Rosen PP, Dershaw DD, Liberman L, Abramson AF. Pseudoangiomatous stromal hyperplasia: mammographic, sonographic, and clinical patterns. Radiology. 1996. 198:117–120.
Article3. Goel NB, Knight TE, Pandey S, Riddick-Young M, de Paredes ES, Trivedi A. Fibrous lesions of the breast: imaging-pathologic correlation. Radiographics. 2005. 25:1547–1559.
Article4. Mercado CL, Naidrich SA, Hamele-Bena D, Fineberg SA, Buchbinder SS. Pseudoangiomatous stromal hyperplasia of the breast: sonographic features with histopathologic correlation. Breast J. 2004. 10:427–432.
Article5. Mendelson EB, Baum JK, Berg WA, Merritt CR, Rubin E. . Ultrasound. Breast Imaging Reporting and Data System (BI-RADS). 2003. 4th ed. Reston, Va: American College of Radiology.6. Powell CM, Cranor ML, Rosen PP. Pseudoangiomatous stromal hyperplasia (PASH). A mammary stromal tumor with myofibroblastic differentiation. Am J Surg Pathol. 1995. 19:270–277.7. Brogi E. Benign and malignant spindle cell lesions of the breast. Semin Diagn Pathol. 2004. 21:57–64.
Article8. Piccoli CW, Feig SA, Palazzo JP. Developing asymmetric breast tissue. Radiology. 1999. 211:111–117.
Article9. Rosen PP. Rosen PP, editor. Benign mesenchymal neoplasms. Rosen's breast pathology. 1997. Philidelphia, PA: Lippincott Raven.10. Polger MR, Denison CM, Lester S, Meyer JE. Pseudoangiomatous stromal hyperplasia: mammographic and sonographic appearances. AJR Am J Roentgenol. 1996. 166:349–352.
Article11. Aron M, Ray R, Verma K. Pseudoangiomatous stromal hyperplasia of the breast-cytological features of two cases and review of literature. Indian J Pathol Microbiol. 2005. 48:260–264.12. Levine PH, Nimeh D, Guth AA, Cangiarella JF. Aspiration biopsy of nodular pseudoangiomatous stromal hyperplasia of the breast: clinicopathologic correlates in 10 cases. Diagn Cytopathol. 2005. 32:345–350.
Article13. Lui PC, Law BK, Chu WC, Pang LM, Tse GM. Fine-needle aspiration cytology of pseudoangiomatous stromal hyperplasia of the breast. Diagn Cytopathol. 2004. 30:353–355.
Article14. Spitz DJ, Reddy VB, Gattuso P. Fine-needle aspiration of pseudoangiomatous stromal hyperplasia of the breast. Diagn Cytopathol. 1999. 20:323–324.
Article15. Hoda SA, Rosen PP. Observations on the pathologic diagnosis of selected unusual lesions in needle core biopsies of breast. Breast J. 2004. 10:522–527.
Article16. Tagaya N, Nakagawa A, Ishikawa Y, Oyama T, Kubota K. Experience with ultrasonographically guided vacuum-assisted resection of benign breast tumors. Clin Radiol. 2008. 63:396–400.
Article17. Ibrahim RE, Sciotto CG, Weidner N. Pseudoangiomatous hyperplasia of mammary stroma. Some observations regarding its clinicopathologic spectrum. Cancer. 1989. 63:1154–1160.
Article18. Sng KK, Tan SM, Mancer JF, Tay KH. The contrasting presentation and management of pseudoangiomatous stromal hyperplasia of the breast. Singapore Med J. 2008. 49:e82–e85.19. Pruthi S, Reynolds C, Johnson RE, Gisvold JJ. Tamoxifen in the management of pseudoangiomatous stromal hyperplasia. Breast J. 2001. 7:434–439.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pseudoangiomatous Stromal Hyperplasia of the Breast Appearing as a Giant Mass: A Case Report
- Mass Forming Pseudoangiomatous Stromal Hyperplasia of the Breast: Sonographic Features
- Rapidly Growing Bilateral Pseudoangiomatous Stromal Hyperplasia of the Breast
- Radiologic Imaging Findings of Bilateral Infiltrating Pseudoangiomatous Stromal Hyperplasia of the Breasts: A Case Report
- Huge Bilateral Breast Hamartoma Accompanied with Pseudoangiomatous Stromal Hyperplasia