Yonsei Med J.
2007 Aug;48(4):671-677. 10.3349/ymj.2007.48.4.671.
The Usefulness of Fetal MRI for Prenatal Diagnosis
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Yonsei University College of Medicine, Seoul, Korea. ywparkob@yuhs.ac
- 2Department of Radiology, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2158174
- DOI: http://doi.org/10.3349/ymj.2007.48.4.671
Abstract
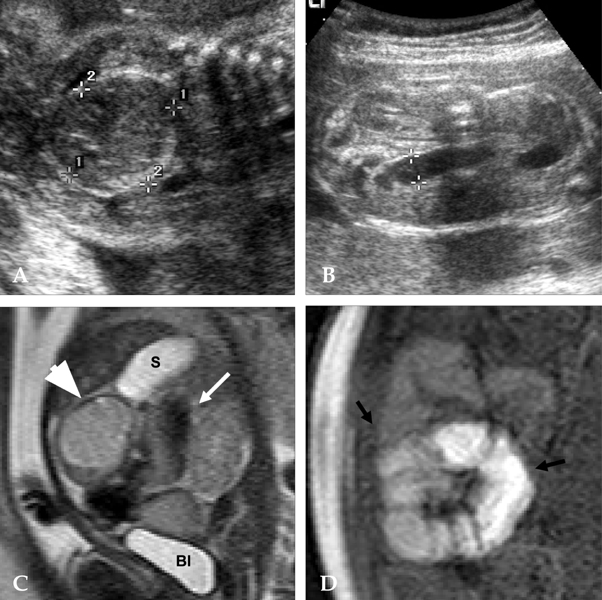
- PURPOSE
Fast MRI has provided detailed and reproducible fetal anatomy. This study was performed to evaluate the usefulness of fetal MRI for prenatal diagnosis. MATERIALS AND METHODS: Fifty-six fetuses with congenital abnormalities on ultrasonography were evaluated by fetal MRI from 2001 to 2004 in Severance Hospital. Final diagnosis was made by postnatal pathology, postnatal MRI, and other modalities (such as ultrasound, retrograde pyelogram). A 1.5-Tesla superconductive MR imaging unit was used to obtain half-Fourier acquisition single-shot turbo spin images. RESULTS: Of the 56 fetuses, intracranial abnormalities were found in 26 fetuses, intraabdominal abnormalities in 17 fetuses, intrathoracic in 6 fetuses, head and neck in 5 fetuses, and other sites in 2 fetuses. There were six cases in which the diagnoses of fetal MRI and ultrasonography differed. In such cases, fetal MRI provided more exact diagnosis than ultrasonography (5 vs. 0). Three fetuses with intracranial abnormalities on ultrasonography were diagnosed as normal by fetal MRI and in postnatal diagnosis. CONCLUSION: Although ultrasonography is known as a screening modality of choice in the evaluation of fetus because of the cost-effectiveness and safety, the sonographic findings are occasionally inconclusive or insufficient for choosing the proper management. Thus, in this study, we suggest that fetal MRI is more useful than ultrasonography for the evaluation of intracranial abnormalities in some instances. For prenatal counseling and postnatal treatment planning, fetal MRI can be informative when prenatal ultrasonography is inadequate and doubtful.
MeSH Terms
Figure
Reference
-
1. Garel C, Brisse H, Sebag G, Elmaleh M, Oury JF, Hassan M. Magnetic resonance imaging of the fetus. Pediatr Radiol. 1998. 28:201–211.
Article2. Angtuaco TL, Shah HR, Mattison DR, Quirk JG. MR imaging in high-risk obstetric patients: a valuable complement to US. Radiographics. 1992. 12:91–110.
Article3. Sonigo PC, Rypens FF, Carteret M, Delezoide AL, Brunelle FO. MR imaging of fetal cerebral anomalies. Pediatr Radiol. 1998. 28:212–222.
Article4. Smith FW, Adam AH, Phillips WD. NMR imaging in pregnancy. Lancet. 1983. 1:61–62.
Article5. Stark DD, McCarthy SM, Filly RA, Parer JT, Hricak H, Callen PW. Pelvimetry by magnetic resonance imaging. AJR Am J Roentgenol. 1985. 144:947–950.
Article6. Yuh WT, Nguyen HD, Fisher DJ, Tali ET, Gao F, Simonson TM, et al. MR of fetal central nervous system abnormalities. AJNR Am J Neuroradiol. 1994. 15:459–464.7. Levine D, Barnes PD, Sher S, Semelka RC, Li W, McArdle CR, et al. Fetal fast MR imaging: reproducibility, technical quality, and conspicuity of anatomy. Radiology. 1998. 206:549–554.
Article8. Hubbard AM. Ultrafast fetal MRI and prenatal diagnosis. Semin Pediatr Surg. 2003. 12:143–153.
Article9. Ertl-Wagner B, Lienemann A, Strauss A, Reiser MF. Fetal magnetic resonance imaging: indications, technique, anatomical considerations and a review of fetal abnormalities. Eur Radiol. 2002. 12:1931–1940.
Article10. Wolff S, Crooks LE, Brown P, Howard R, Painter R. Tests for DNA and chromosomal damage induced by nuclear magnetic resonance imaging. Radiology. 1980. 136:707–710.
Article11. Schwartz JL, Crooks LE. NMR imaging produces no observable mutations or cytotoxicity in mammalian cells. AJR Am J Roentgenol. 1982. 139:583–585.
Article12. Kanal E, Gillen J, Evans JA, Savitz DA, Shellock FG. Survey of reproductive health among female MR workers. Radiology. 1993. 187:395–399.
Article13. Baker PN, Johnson IR, Harvey PR, Gowland PA, Mansfield P. A three-year follow-up of children imaged in utero with echo-planar magnetic resonance. Am J Obstet Gynecol. 1994. 170:32–33.
Article14. Shellock FG, Kanal E. Policies, guidelines, and recommendations for MR imaging safety and patient management. SMRI safety Committee. J Magn Reson Imaging. 1991. 1:97–101.
Article15. Shellock FG, Kanal E. Edelman RR, Hesselink JR, Zlatkin MB, editors. Bioeffects and safety of MR procedures. Clinical magnetic resonance imaging. 1996. 2nd ed. Philadelphia: Saunders;429.16. Hubbard AM, Harty MP, States LJ. A new tool for prenatal diagnosis: ultrafast fetal MRI. Semin Perinatol. 1999. 23:437–447.
Article17. Blaicher W, Prayer D, Bernaschek G. Magnetic resonance imaging and ultrasound in the assessment of the fetal central nervous system. J Perinat Med. 2003. 31:459–468.
Article18. Pretorius DH, Davis K, Manco-Johnson ML, Manchester D, Meier PR, Clewell WH. Clinical course of fetal hydrocephalus: 40 cases. AJR Am J Roentgenol. 1985. 144:827–831.
Article19. Nyberg DA, Mack LA, Hirsch J, Pagon RO, Shepard TH. Fetal hydrocephalus: sonographic detection and clinical significance of associated anomalies. Radiology. 1987. 163:187–191.
Article20. Vintzileos AM, Campbell WA, Weinbaum PJ, Nochimson DJ. Perinatal management and outcome of fetal ventriculomegaly. Obstet Gynecol. 1987. 69:5–11.21. Cochrane DD, Myles ST, Nimrod C, Still DK, Sugarman RG, Wittmann BK. Intrauterine hydrocephalus and ventriculomegaly: associated anomalies and fetal outcome. Can J Neurol Sci. 1985. 12:51–59.
Article22. Chervenak FA, Duncan C, Ment LR, Hobbins JC, McClure M, Scott D, et al. Outcome of fetal ventriculomegaly. Lancet. 1984. 2:179–181.
Article23. Levine D. Fetal magnetic resonance imaging. J Matern Fetal Neonatal Med. 2004. 15:85–94.
Article24. Benachi A, Sonigo P, Jouannic JM, Simon I, Rvillon Y, Brunelle F, et al. Determination of anatomical location of an antenatal intestinal occlusion by magnetic resonance imaging. Ultrasound Obstet Gynecol. 2001. 18:163–165.
Article25. Hubbard AM, Crombleholme TM, Adzick NS. Prenatal MRI evaluation of giant neck masses in preparation for the fetal exit procedure. Am J Perinatol. 1998. 15:253–257.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of fetal magnetic resonance imaging and ultrasonography for the diagnosis of fetal anomalies
- Imaging Diagnosis of Fetal Abdominal Solid Tumor
- Two Cases of Fetal Arachnoid Cyst Diagnosed by Prenatal Ultrasonography
- The Clinical Importance of the Prenatal Diagnosis of Fetal Scalp Hemangioma
- Recent Trends in Prenatal Diagnosis of Fetal Malformations