Yonsei Med J.
2005 Oct;46(5):652-657. 10.3349/ymj.2005.46.5.652.
Uterine Artery Doppler Velocimetry During Mid-second Trimester to Predict Complications of Pregnancy Based on Unilateral or Bilateral Abnormalities
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Yonsei University College of Medicine, Seoul, Korea. 28543@kuh.ac.kr
- KMID: 2158145
- DOI: http://doi.org/10.3349/ymj.2005.46.5.652
Abstract
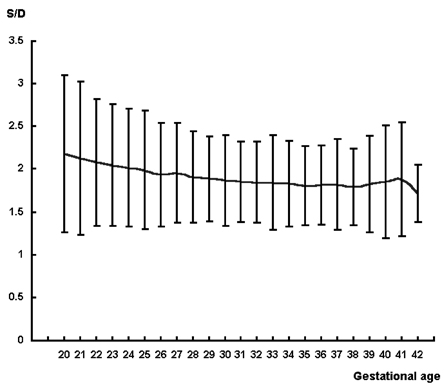
- We performed this study to evaluate uterine artery Doppler velocimetry (UADV) measurement of unilateral or bilateral abnormalities as a predictor of complications in pregnancy during the mid-second trimester (20-24 weeks). We enrolled 1, 090 pregnant women who had undergone UADV twice: once between the 20th and 24th week (1st stage) and again between the 28th and 32nd week (2nd stage) of pregnancy, and then delivered at Yonsei Medical Center. UADV was performed bilaterally. Follow-up UADV was performed between the 28th and 32nd week, and the frequencies of pregnancy-induced hypertension (PIH), fetal growth restriction (FGR), and preterm delivery (before 34 weeks of gestation) were determined. Chi-squared and t-tests were used where appropriate, with p < .05 considered significant. According to the results of UADV performed between 20-24 weeks of gestation, 825 women (75.7%) were included in the normal group, 196 (18.0%) in the unilateral abnormality group, and 69 (6.3%) in the bilateral abnormality group. The incidences of FGR were 8.0%, 10.2%, and 26.1%, and the incidences of PIH were 0.1%, 3.6%, and 14.5%, respectively. The incidence of PIH was significantly lower in the normal group. The incidences of preterm delivery were 2.2%, 5.6%, and 8.7%, respectively. PIH developed in 46.7% of patients with bilateral abnormal findings in both the 1st and 2nd stage tests, and developed in none of the patients with normal findings in both tests. Abnormal results found by UADV performed between the 20-24th weeks of pregnancy, such as high S/D ratios regardless of placental location and the presence of an early diastolic notch, were associated with significant increases in the incidences of intrauterine growth restriction (IUGR) and PIH. This was true for both bilateral and unilateral abnormalities. Abnormal findings in bilateral UADV during the second trimester especially warrant close follow up for the detection of subsequent development of pregnancy complications.
Keyword
MeSH Terms
Figure
Reference
-
1. Committee on Practice Bulletins--Gynecology, American College of Obstetricians and Gynecologists, Washington, DC 20090-6920, USA. Intrauterine growth restriction. Clinical management guidelines for obstetrician-gynecologists. American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet. 2001. 72:85–96.2. Gladstone IM, Katz VL. The morbidity of the 34- to 35-week gestation: should we reexamine the paradigm? Am J Perinatol. 2004. 21:9–13.3. Meekins JW, Pijnenborg R, Hanssens M, McFayden IR, van Assche A. A study of placental bed spiral arteries and trophoblast invasion in normal and severe pre-eclamptic pregnancies. Br J Obstet Gynaecol. 1994. 101:669–674.4. Browne JC, Veall N. The maternal placental blood flow in normotensive and hypertensive women. J Obstet Gynecol Br Emp. 1953. 60:141–147.5. Campbell S, Diaz-Recasens J, Griffin DR, Cohen-Overbeek TE, Pearce JM, Wilson K, et al. New Doppler technique for assessing uteroplacental blood flow. Lancet. 1983. 1:675–677.6. Strigini FA, Lencioni G, De Luca G, Lombardo M, Bianchi F, Genazzani AR. Uterine artery velocimetry and spontaneous preterm delivery. Obstet Gynecol. 1995. 85:374–377.7. Albaiges G, Missfelder-Lobos H, Lees C, Parra M, Nicolaides KH. One-stage screening for pregnancy complications by color Doppler assessment of the uterine arteries at 23 weeks' gestation. Obstet Gynecol. 2000. 96:559–564.8. Phupong V, Dejthevaporn T, Tanawattanacharoen S, Manotaya S, Tannirandorn Y, Charoenvidhya D. Predicting the risk of preeclampsia and small for gestational age infants by uterine artery Doppler in low-risk women. Arch Gynecol Obstet. 2003. 268:158–161.9. Benedetto C, Valensise H, Marozio L, Giarola M, Massobrio M, Romanini C. A two-stage screening test for pregnancy-induced hypertension and preeclampsia. Obstet Gynecol. 1998. 92:1005–1011.10. Campbell S, Pearce JM, Hackett G, Cohen-Overbeek T, Hernandez C. Qualitative assessment of uteroplacental blood flow: early screening test for high-risk pregnancies. Obstet Gynecol. 1986. 68:649–653.11. Jacobson SL, Imhof R, Manning N, Mannion V, Little D, Rey E, et al. The value of Doppler assessment of the uteroplacental circulation in predicting preeclampsia or intrauterine growth retardation. Am J Obstet Gynecol. 1990. 162:110–114.12. Chung JE, Cho JS, Han SS, Park YW, Kim JW. Uterine artery Doppler velocimetry in the prediction of adverse obstetric outcomes in unexplained MSAFP elevations. Yonsei Med J. 2000. 41:17–21.13. Thaler I, Weiner Z, Itskovitz J. Systolic or diastolic notch in uterine artery blood flow velocity waveforms in hypertensive pregnant patients: relationship to outcome. Obstet Gynecol. 1992. 80:277–282.14. Park YW, Cho JS, Kim HS, Kim JS, Song CH. The clinical implications of early diastolic notch in third trimester Doppler wave form analysis of the uterine artery. J Ultrasound Med. 1996. 15:47–51.15. Davey DA, MacGillivray I. The classification and definition of the hypertensive disorders of pregnancy. Am J Obstet Gynecol. 1988. 158:892–898.16. Park YW, Cho JS, Han SS, Kim JW. Clinical significance of early diastolic notch of uterine artery Doppler velocimetry in relation to placental location. Korean J Obstet Gynecol. 1999. 42:2486–2491.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Uterine Artery Doppler Velocimetry as a Screening Test in the Second Trimester Pregnancies
- Uterine artery Doppler velocimetry in the prediction of adverse obstetric outcomes in unexplained MSAFP elevations
- The Relationship of Early Diastolic Notch in Uterine Artery Doppler Velocimetry and the Renal Function of Patients with Pregnancy Induced Hypertension
- Significance of Uterine Artery Doppler Velocimetry During Midtrimester in Chronic Hypertensive Patients
- The Prediction of Pre-eclampsia/Fetal Growth Restriction based on Notch of Uterine Artery Doppler Velocimetry