Korean J Radiol.
2015 Jun;16(3):541-549. 10.3348/kjr.2015.16.3.541.
Diagnostic Performance of CT Angiography in Patients Visiting Emergency Department with Overt Gastrointestinal Bleeding
- Affiliations
-
- 1Department of Radiology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Institute of Radiation Medicine, Seoul National University Medical Research Center, Seongnam 436-707, Korea. yhkrad@gmail.com
- KMID: 2155523
- DOI: http://doi.org/10.3348/kjr.2015.16.3.541
Abstract
OBJECTIVE
To investigate the diagnostic performance of computed tomography angiography (CTA) in identifying the cause of bleeding and to determine the clinical features associated with a positive test result of CTA in patients visiting emergency department with overt gastrointestinal (GI) bleeding.
MATERIALS AND METHODS
We included 111 consecutive patients (61 men and 50 women; mean age: 63.4 years; range: 28-89 years) who visited emergency department with overt GI bleeding. They underwent CTA as a first-line diagnostic modality from July through December 2010. Two radiologists retrospectively reviewed the CTA images and determined the presence of any definite or potential bleeding focus by consensus. An independent assessor determined the cause of bleeding based on other diagnostic studies and/or clinical follow-up. The diagnostic performance of CTA and clinical characteristics associated with positive CTA results were analyzed.
RESULTS
To identify a definite or potential bleeding focus, the diagnostic yield of CTA was 61.3% (68 of 111). The overall sensitivity, specificity, positive predictive value (PPV), and negative predictive value were 84.8% (67 of 79), 96.9% (31 of 32), 98.5% (67 of 68), and 72.1% (31 of 43), respectively. Positive CTA results were associated with the presence of massive bleeding (p = 0.001, odds ratio: 11.506).
CONCLUSION
Computed tomography angiography as a first-line diagnostic modality in patients presenting with overt GI bleeding showed a fairly high accuracy. It could identify definite or potential bleeding focus with a moderate diagnostic yield and a high PPV. CTA is particularly useful in patients with massive bleeding.
MeSH Terms
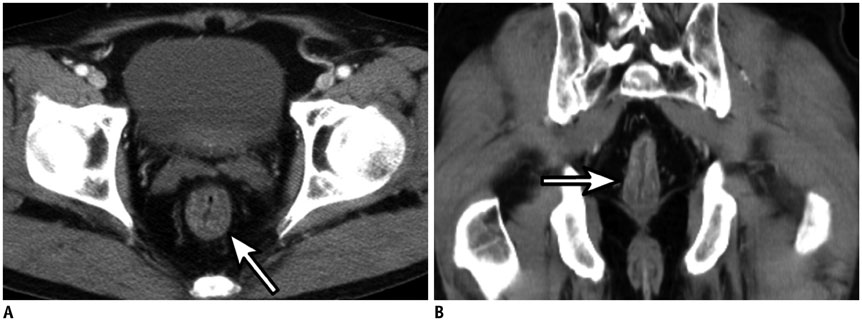
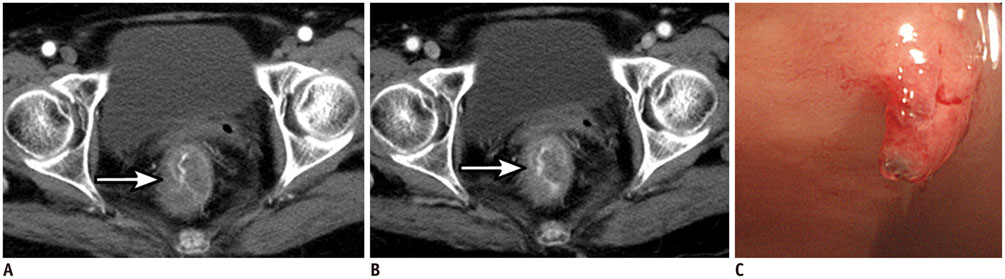
Figure
Reference
-
1. Zuckerman GR, Prakash C, Askin MP, Lewis BS. AGA technical review on the evaluation and management of occult and obscure gastrointestinal bleeding. Gastroenterology. 2000; 118:201–221.2. Barnert J, Messmann H. Diagnosis and management of lower gastrointestinal bleeding. Nat Rev Gastroenterol Hepatol. 2009; 6:637–646.3. Kennedy DW, Laing CJ, Tseng LH, Rosenblum DI, Tamarkin SW. Detection of active gastrointestinal hemorrhage with CT angiography: a 4(1/2)-year retrospective review. J Vasc Interv Radiol. 2010; 21:848–855.4. van Leerdam ME, Vreeburg EM, Rauws EA, Geraedts AA, Tijssen JG, Reitsma JB, et al. Acute upper GI bleeding: did anything change? Time trend analysis of incidence and outcome of acute upper GI bleeding between 1993/1994 and 2000. Am J Gastroenterol. 2003; 98:1494–1499.5. Strate LL, Naumann CR. The role of colonoscopy and radiological procedures in the management of acute lower intestinal bleeding. Clin Gastroenterol Hepatol. 2010; 8:333–343. quiz e44.6. Frattaroli FM, Casciani E, Spoletini D, Polettini E, Nunziale A, Bertini L, et al. Prospective study comparing multi-detector row CT and endoscopy in acute gastrointestinal bleeding. World J Surg. 2009; 33:2209–2217.7. Jensen DM, Machicado GA, Jutabha R, Kovacs TO. Urgent colonoscopy for the diagnosis and treatment of severe diverticular hemorrhage. N Engl J Med. 2000; 342:78–82.8. Whelan CT, Chen C, Kaboli P, Siddique J, Prochaska M, Meltzer DO. Upper versus lower gastrointestinal bleeding: a direct comparison of clinical presentation, outcomes, and resource utilization. J Hosp Med. 2010; 5:141–147.9. Martí M, Artigas JM, Garzón G, Alvarez-Sala R, Soto JA. Acute lower intestinal bleeding: feasibility and diagnostic performance of CT angiography. Radiology. 2012; 262:109–116.10. Lee SS, Oh TS, Kim HJ, Chung JW, Park SH, Kim AY, et al. Obscure gastrointestinal bleeding: diagnostic performance of multidetector CT enterography. Radiology. 2011; 259:739–748.11. Jaeckle T, Stuber G, Hoffmann MH, Jeltsch M, Schmitz BL, Aschoff AJ. Detection and localization of acute upper and lower gastrointestinal (GI) bleeding with arterial phase multidetector row helical CT. Eur Radiol. 2008; 18:1406–1413.12. Yoon W, Jeong YY, Shin SS, Lim HS, Song SG, Jang NG, et al. Acute massive gastrointestinal bleeding: detection and localization with arterial phase multi-detector row helical CT. Radiology. 2006; 239:160–167.13. García-Blázquez V, Vicente-Bártulos A, Olavarria-Delgado A, Plana MN, van der Winden D, Zamora J, et al. Accuracy of CT angiography in the diagnosis of acute gastrointestinal bleeding: systematic review and meta-analysis. Eur Radiol. 2013; 23:1181–1190.14. Pennazio M, Santucci R, Rondonotti E, Abbiati C, Beccari G, Rossini FP, et al. Outcome of patients with obscure gastrointestinal bleeding after capsule endoscopy: report of 100 consecutive cases. Gastroenterology. 2004; 126:643–653.15. Geffroy Y, Rodallec MH, Boulay-Coletta I, Jullès MC, Ridereau-Zins C, Zins M. Multidetector CT angiography in acute gastrointestinal bleeding: why, when, and how. Radiographics. 2011; 31:E35–E46.16. Lefkovitz Z, Cappell MS, Kaplan M, Mitty H, Gerard P. Radiology in the diagnosis and therapy of gastrointestinal bleeding. Gastroenterol Clin North Am. 2000; 29:489–512.17. Ernst O, Bulois P, Saint-Drenant S, Leroy C, Paris JC, Sergent G. Helical CT in acute lower gastrointestinal bleeding. Eur Radiol. 2003; 13:114–117.18. Yoon W, Jeong YY, Kim JK. Acute gastrointestinal bleeding: contrast-enhanced MDCT. Abdom Imaging. 2006; 31:1–8.19. Duchesne J, Jacome T, Serou M, Tighe D, Gonzales A, Hunt JP, et al. CT-angiography for the detection of a lower gastrointestinal bleeding source. Am Surg. 2005; 71:392–397.20. Miller FH, Hwang CM. An initial experience: using helical CT imaging to detect obscure gastrointestinal bleeding. Clin Imaging. 2004; 28:245–251.21. Velayos FS, Williamson A, Sousa KH, Lung E, Bostrom A, Weber EJ, et al. Early predictors of severe lower gastrointestinal bleeding and adverse outcomes: a prospective study. Clin Gastroenterol Hepatol. 2004; 2:485–490.22. Stuhlfaut JW, Soto JA, Lucey BC, Ulrich A, Rathlev NK, Burke PA, et al. Blunt abdominal trauma: performance of CT without oral contrast material. Radiology. 2004; 233:689–694.23. Khamaysi I, Gralnek IM. Acute upper gastrointestinal bleeding (UGIB) - initial evaluation and management. Best Pract Res Clin Gastroenterol. 2013; 27:633–638.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiologic Diagnosis of Gastrointestinal Bleeding
- Role of computed tomography angiography for acute gastrointestinal bleeding
- Diagnostic accuracy and implementation of computed tomography angiography for gastrointestinal hemorrhage according to clinical severity
- The Usefulness of MDCT in Acute Intestinal Bleeding
- Provocative mesenteric angiography for diagnosis and treatment of occult gastrointestinal hemorrhage