J Korean Soc Radiol.
2016 Mar;74(3):189-194. 10.3348/jksr.2016.74.3.189.
Primary Hepatic Mucosa-Associated Lymphoid Tissue Lymphoma: A Case Report
- Affiliations
-
- 1Department of Radiology, Daejin Medical Center Bundang Jesaeng General Hospital, Seongnam, Korea. neverendlove@hanmail.net
- 2Department of Pathology, Daejin Medical Center Bundang Jesaeng General Hospital, Seongnam, Korea.
- 3Department of Internal Medicine, Daejin Medical Center Bundang Jesaeng General Hospital, Seongnam, Korea.
- KMID: 2155279
- DOI: http://doi.org/10.3348/jksr.2016.74.3.189
Abstract
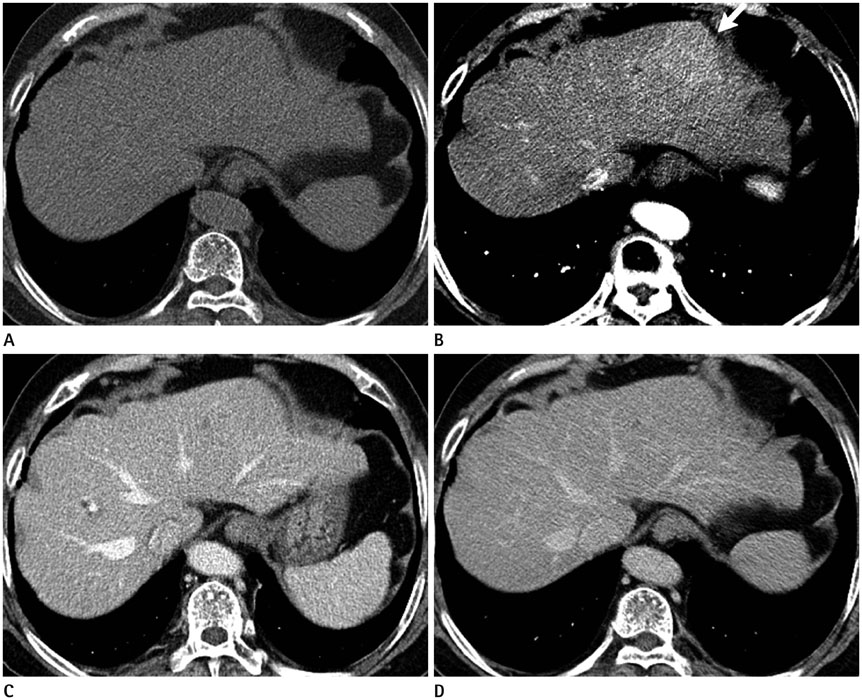
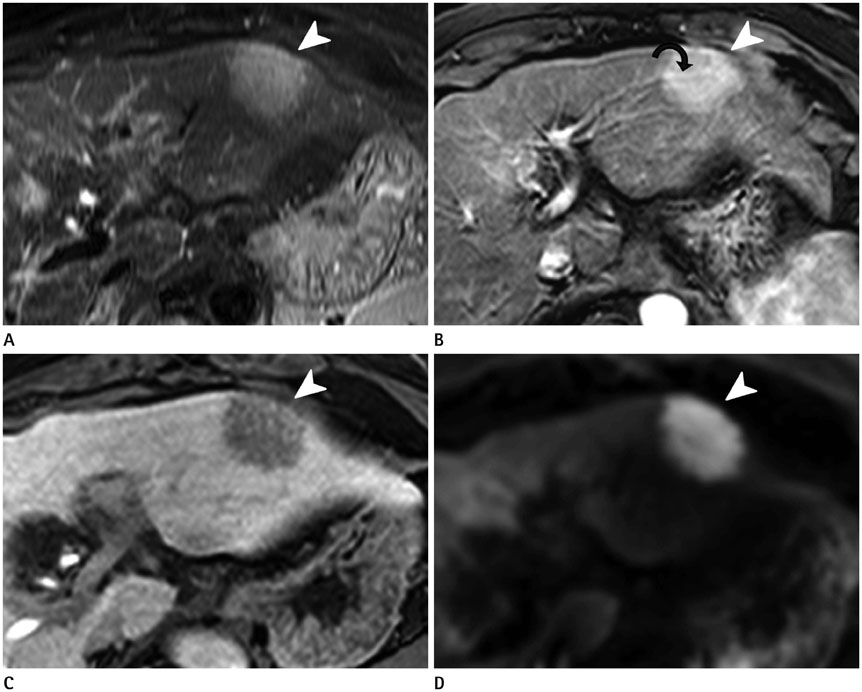
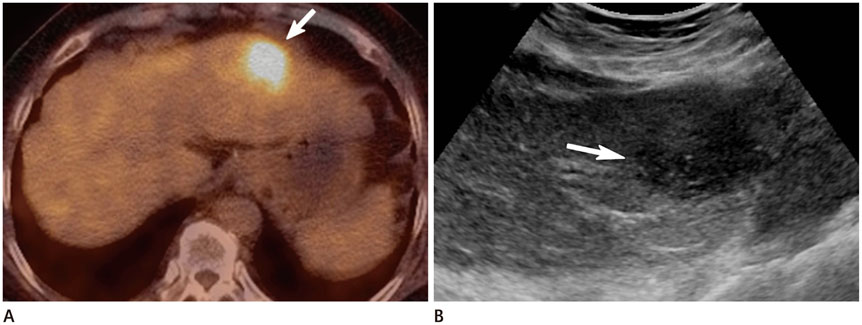
- Primary hepatic mucosa-associated lymphoid tissue (MALT) lymphoma is an extremely rare lesion. Primary hepatic lymphomas are known to present as a single mass in > 70% of cases, and in many instances with no specific features on imaging. Herein, we described a case of primary hepatic MALT lymphoma in a 71-year-old woman. A computed tomography (CT) scan revealed a mass, 4.5 x 3.0 cm, in liver segment 2 (S2) that was poorly defined, with subtle enhancement during the arterial phase. Gadoxetic acid-enhanced magnetic resonance imaging also showed an arterially enhancing mass in S2, with low signal intensity during the hepatobiliary phase and high signal intensity on diffusion-weighted imaging with a high b-value. On fluorodeoxyglucose positron emission tomography/CT imaging, the mass showed a high standardized uptake value. Ultrasonography (US) revealed a hypoechoic mass, and US-guided core needle biopsy confirmed a hepatic MALT lymphoma.
MeSH Terms
Figure
Reference
-
1. Matasar MJ, Zelenetz AD. Overview of lymphoma diagnosis and management. Radiol Clin North Am. 2008; 46:175–198, vii.2. Isaacson P, Wright DH. Malignant lymphoma of mucosa-associated lymphoid tissue. A distinctive type of B-cell lymphoma. Cancer. 1983; 52:1410–1416.3. Park JY, Choi MS, Lim YS, Park JW, Kim SU, Min YW, et al. Clinical features, image findings, and prognosis of inflammatory pseudotumor of the liver: a multicenter experience of 45 cases. Gut Liver. 2014; 8:58–63.4. Doi H, Horiike N, Hiraoka A, Koizumi Y, Yamamoto Y, Hasebe A, et al. Primary hepatic marginal zone B cell lymphoma of mucosa-associated lymphoid tissue type: case report and review of the literature. Int J Hematol. 2008; 88:418–423.5. Grazioli L, Olivetti L, Mazza G, Bondioni MP. MR imaging of hepatocellular adenomas and differential diagnosis dilemma. Int J Hepatol. 2013; 2013:374170.6. Apicella PL, Mirowitz SA, Weinreb JC. Extension of vessels through hepatic neoplasms: MR and CT findings. Radiology. 1994; 191:135–136.7. Jaffe ES. Malignant lymphomas: pathology of hepatic involvement. Semin Liver Dis. 1987; 7:257–268.8. Rodallec M, Guermazi A, Brice P, Attal P, Zagdanski AM, Frija J, et al. Imaging of MALT lymphomas. Eur Radiol. 2002; 12:348–356.9. Shiozawa K, Watanabe M, Ikehara T, Matsukiyo Y, Kikuchi Y, Kaneko H, et al. A case of contiguous primary hepatic marginal zone B-cell lymphoma and hemangioma ultimately diagnosed using contrast-enhanced ultrasonography. Case Rep Oncol. 2015; 8:50–56.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Longlasting Remission of Primary Hepatic Mucosa-associated Lymphoid Tissue (MALT) Lymphoma Achieved by Radiotherapy Alone
- Mucosa-Associated Lymphoid Tissue Lymphoma of the Esophagus Coexistent with Bronchus-Associated Lymphoid Tissue Lymphoma of the Lung
- Primary Mucosa-Associated Lymphoid Tissue Lymphoma of the Breast with Synchronous Contralateral Invasive Breast Cancer: A Case Report
- A case report of the Pulmonary Malignant Lymphomaof the mucosa-associated lymphoid tissue(MALT)
- Mucosa-Associated Lymphoid Tissue Lymphoma Arising from the Nasal Mucosa: A Case Report and Review of the Literature