Kosin Med J.
2015 Dec;30(2):123-130. 10.7180/kmj.2015.30.2.123.
Complications caused by perfluorocarbon liquid used in pars plana vitrectomy
- Affiliations
-
- 1Oksan Health Subcenter, Euiseong-Gun, Korea.
- 2Department of Ophthalmology, College of Medicine, Kosin University, Busan, Korea. hhiatus@gmail.com
- KMID: 2150498
- DOI: http://doi.org/10.7180/kmj.2015.30.2.123
Abstract
OBJECTIVES
To assess the inadvertent intraocular retention of perfluorocarbon liquid (PFCL) after vitreoretinal surgery and their complications.
METHODS
We retrospectively reviewed the medical records of 108 patients who underwent vitreoretinal surgeries using intraoperative PFCL (perfluoro-n-octane (C8F18), 0.69 centistoke at 25degrees C, PERFLUORN(R), Alcon, USA) and the removal of PFCL through fluid-air exchange. The analysis was focused on the occurrence of intraocular retained PFCL, diagnoses,surgicalprocedures,andcomplications.
RESULTS
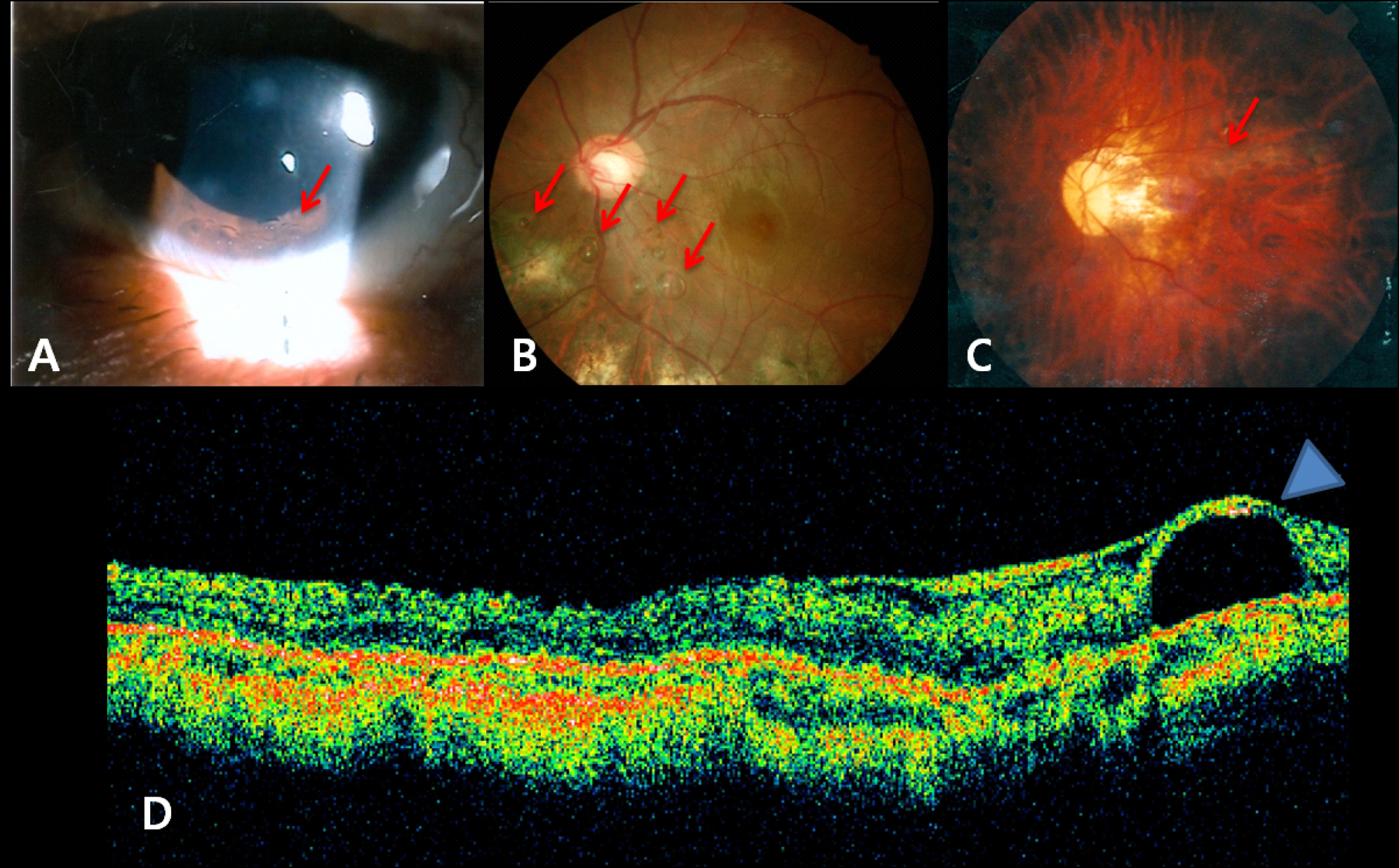
Retinal detachment (51 cases, 47%) was the most common surgery which used PFCL intraoperatively. Other causes were vitreous hemorrhage (24 cases, 22%), posteriorly dislocated lens (22 cases, 21%), and trauma (11 cases, 10%). Intraocular PFCL was found in a total of 9 (8.3%) eyes. PFCL bubbles remained in anterior chamber and vitreous cavity were observed in 4 cases and subretinal retained PFCL was observed in 5 cases. Three of 5 cases of subretinal PFCL exhibited in subfoveal space. Among the three subfoveal cases, macular hole developed after PFCL removal in 1 case, epiretinal membrane in the area where had been PFCL bubble. However, we observed no complications in 1 case of subfoveal PFCL that was removed by surgery. PFCL in anterior chamber and vitreous cavity were in 4 cases.
CONCLUSIONS
The presence of subfoveal PFCL might affect visual and anatomic outcomes. However, subfoveal PFCL may induce visual complications, and therefore requires special attention.
MeSH Terms
Figure
Reference
-
References
1. Lesnoni G, Rossi T, Gelso A. Subfoveal liquid perfluorocarbon. Retina. 2004; 24:172–6.
Article2. Chang S, Lincoff H, Zimmerman NJ, Fuchs W. Giant retinal tears. Surgical techniques and results using perfluorocarbon liquids. Arch Ophthalmol. 1989; 107:761–6.3. Peyman GA, Schulman JA, Sullivan B. Perfluorocarbon liquids in ophthalmology. Surv Ophthalmol. 1995; 39:375–95.4. Han DP, Nanda SK, O'Brien WJ, Guy J, Murray TG, Boldt HC. Evaluation of anterior segment tolerance to short-term intravitreal perfluoron. Retina. 1994; 14:219–24.
Article5. Tanji TM, Peyman GA, Mehta NJ, Millsap CM. Perfluoroperhydrophenanthrene (Vitreon) as a short-term vitreous substitute after complex vitreoretinal surgery. Ophthalmic surgery. 1993; 24:681–5.
Article6. Garcia-Valenzuela E, Ito Y, Abrams GW. Risk factors for retention of subretinal perfluorocarbon liquid in vitreoretinal surgery. Retina. 2004; 24:746–52.
Article7. Bourke RD, Simpson RN, Cooling RJ, Sparrow JR. The stability of perfluoro-N-octane during vitreoretinal procedures. Archives of ophthalmology. 1996; 114:537–44.
Article8. Scott IU, Murray TG, Flynn HW, Jr. , Smiddy WE, Feuer WJ, Schiffman JC. Outcomes and complications associated with perfluoro-n-octane and perfluoroperhydrophenanthrene in complex retinal detachment repair. Ophthalmology. 2000; 107:860–5.
Article9. Viebahn M, Buettner H. Perfluorophenanthrene unsuitable for postoperative retinal tamponade. Am J Ophthalmol. 1994; 118:124–6.
Article10. Moreira H, de Queiroz JM, Jr. , Liggett PE, McDonnell PJ. Corneal toxicity study of two perfluorocarbon liquids in rabbit eyes. Cornea. 1992; 11:376–9.
Article11. Alster Y, Ben-Nun Y, Loewenstein A, Lazar M. Pupillary block glaucoma due to residual perfluorodecalin. Ophthalmic Surg Lasers. 1996; 27:395–6.
Article12. Aydin E, Demir HD. Perfluorodecaline residue in the anterior chamber of a patient with an intact crystalline lens: a case report. J Med Case Rep. 2008; 2:13.
Article13. Wilbanks GA, Apel AJ, Jolly SS, Devenyi RG, Rootman DS. Perfluorodecalin corneal toxicity: five case reports. Cornea. 1996; 15:329–34.
Article14. Rofail M, Lee LR. Perfluoro-n-octane as a postoperative vitreoretinal tamponade in the management of giant retinal tears. Retina. 2005; 25:897–901.
Article15. Eckardt C, Nicolai U, Winter M, Knop E. Experimental intraocular tolerance to liquid perfluorooctane and perfluoropolyether. Retina. 1991; 11:375–84.
Article16. Vilaplana D, Poposki V, Martinez-Palmer A, Castilla M. [Subfoveal perfluorocarbon liquid. Two new cases]. Arch Soc Esp Oftalmol. 2009; 84:363–6.17. Escalada Gutierrez F, Mateo Garcia C. [Extraction of subfoveal liquid perfluorocarbon]. Arch Soc Esp Oftalmol. 2002; 77:519–21.18. Wong TY, Ho T. Retained perfluorodecalin after retinal detachment surgery. Int Ophthalmol. 1996; 20:293–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Trabeculectomy Combined with Pars Plana Vitrectomy
- The Clinical Evaluation of Pars Plana Vitrectomy in various Ocular Disease
- Subretinal Fluid Drainage through Original Breaks without Perfluorocarbon Liquid for Rhegmatogenous Retinal Detachment
- Combined Clear Corneal Phacoemulsification and Pars Plana Vitrectomy
- The Alteration of Accommodative Power after Scleral Buckling and Pars Plana Vitrectomy