Korean J Pain.
2015 Jul;28(3):198-202. 10.3344/kjp.2015.28.3.198.
Effect of Intravenous Intraoperative Esmolol on Pain Management Following Lower Limb Orthopedic Surgery
- Affiliations
-
- 1Anesthesiology Research Center, Guilan University of Medical Sciences, Rasht, Iran.
- 2Orthopedic Research Center, Guilan University of Medical Sciences, Rasht, Iran. ahmadreza.mirbolook@gmail.com
- 3Guilan University of Medical Sciences, Rasht, Iran.
- 4Guilan Trauma Research Center, Guilan University of Medical Sciences, Rasht, Iran.
- 5Qazvin University of Medical Sciences, Qazvin, Iran.
- KMID: 2149464
- DOI: http://doi.org/10.3344/kjp.2015.28.3.198
Abstract
- BACKGROUND
Lack of proper control of acute postoperative pain often leads to lingering or chronic pain. Several studies have emphasized the role of beta-blockers in reducing postoperative pain. Esmolol is a selective short-acting beta-blocker that produces few side effects. The purpose of this study was to examine the effect of intravenous intraoperative esmolol on postoperative pain reduction following orthopedic leg fracture surgery.
METHODS
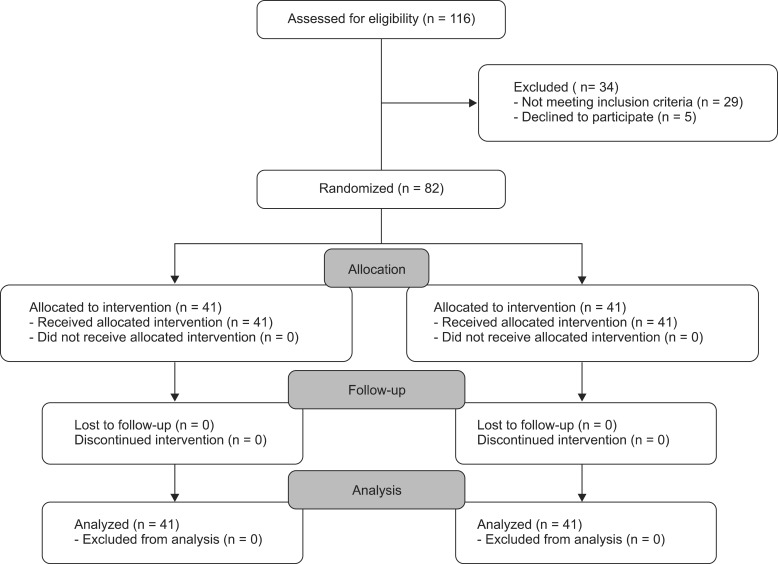
In a clinical trial, 82 patients between 20-65 years of age with tibia fractures and American Society of Anesthesiologists (ASA) physical status I & II who underwent surgery were divided into two groups. Group A received esmolol and group B received normal saline. Postoperative pain was measured at three time points: entering the recovery unit, and at 3 h and 6 h following surgery, using the Visual Analogue Scale (VAS). A P value of < 0.05 was considered significant.
RESULTS
Mean VAS scores at all three time points were significantly different between the two test groups (P = 0.02, P = 0.0001, and P = 0.0001, respectively). The consumption of pethidine was lower in group A than in group B (P = 0.004) and the duration of its effect was significantly longer in time (P = 0.026).
CONCLUSIONS
Intravenous intraoperative esmolol is effective in the reduction of postoperative pain following leg fracture surgery. It reduced opioid consumption following surgery and delayed patient requests for analgesics.
Keyword
MeSH Terms
Figure
Reference
-
1. White PF, Wang B, Tang J, Wender RH, Naruse R, Sloninsky A. The effect of intraoperative use of esmolol and nicardipine on recovery after ambulatory surgery. Anesth Analg. 2003; 97:1633–1638. PMID: 14633533.
Article2. Yang H, Fayad A. Are beta-blockers anesthestics? Can J Anaesth. 2003; 50:627–630. PMID: 12944432.3. Stein C, Kopf A. Anesthesia and treatment of chronic pain. In : Miller R, Eriksson L, Fleisher L, Wiener-Kronish J, Young W, editors. Miller's anesthesia. 7th ed. Philadelphia, PA: Churchill Livingstone;2010. p. 1797–1817.4. Ono H, Ohtani N, Matoba A, Kido K, Yasui Y, Masaki E. Efficacy of intrathecal esmolol on heat-evoked responses in a postoperative pain model. Am J Ther. 2015; 22:111–116. PMID: 23411610.
Article5. Bhawna , Bajwa SJ, Lalitha K, Dhar P, Kumar V. Influence of esmolol on requirement of inhalational agent using entropy and assessment of its effect on immediate postoperative pain score. Indian J Anaesth. 2012; 56:535–541. PMID: 23325937.
Article6. Yu SK, Tait G, Karkouti K, Wijeysundera D, McCluskey S, Beattie WS. The safety of perioperative esmolol: a systematic review and meta-analysis of randomized controlled trials. Anesth Analg. 2011; 112:267–281. PMID: 21127279.7. Lee SJ, Lee JN. The effect of perioperative esmolol infusion on the postoperative nausea, vomiting and pain after laparoscopic appendectomy. Korean J Anesthesiol. 2010; 59:179–184. PMID: 20877702.
Article8. Casalino S, Fabozzi M, Millo P, Cena A, Angellotti A, Albani A. Esmolol vs epidural anesthesia in bariatric surgery: pain control and postoperative outcome: 1AP1-1. Eur J Anaesthesiol. 2011; 28:6–7.
Article9. Coloma M, Chiu JW, White PF, Armbruster SC. The use of esmolol as an alternative to remifentanil during desflurane anesthesia for fast-track outpatient gynecologic laparoscopic surgery. Anesth Analg. 2001; 92:352–357. PMID: 11159231.
Article10. White P, Eng M. Ambulatory (out patient) anesthesia. In : Miller R, Eriksson L, Fleisher L, Wiener-Kronish J, Young W, editors. Miller's anesthesia. 7th ed. Philadelphia, PA: Churchill Livingstone;2010. p. 2426.11. Ozturk T, Kaya H, Aran G, Aksun M, Savaci S. Postoperative beneficial effects of esmolol in treated hypertensive patients undergoing laparoscopic cholecystectomy. Br J Anaesth. 2008; 100:211–214. PMID: 18037672.
Article12. Celebi N, Cizmeci EA, Canbay O. Intraoperative esmolol infusion reduces postoperative analgesic consumption and anaesthetic use during septorhinoplasty: a randomized trial. Rev Bras Anestesiol. 2014; 64:343–349. PMID: 25168439.
Article13. Collard V, Mistraletti G, Taqi A, Asenjo JF, Feldman LS, Fried GM, et al. Intraoperative esmolol infusion in the absence of opioids spares postoperative fentanyl in patients undergoing ambulatory laparoscopic cholecystectomy. Anesth Analg. 2007; 105:1255–1262. PMID: 17959952.
Article14. Stanley TH, de Lange S, Boscoe MJ, de Bruijn N. The influence of chronic preoperative propranolol therapy on cardiovascular dynamics and narcotic requirements during operation in patients with coronary artery disease. Can Anaesth Soc J. 1982; 29:319–324. PMID: 6213289.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effectiveness and Causes of Early Cessation of Intravenous Patient-Controlled Analgesia in Orthopedic Surgery
- Nicardipine is more effective than esmolol at preventing blood pressure increases during emergence from total intravenous anesthesia
- Effects of Hydralazine Pretreatment on Esmolol-induced Controlled Hypotension during Spine Surgery
- The Effect of Cranial Pin Insertion on Blood Pressure and Heart Rate after Injecting Fentanyl and Esmolol or Thiopental Sodium and Esmolol
- Spinal Cauda Equina Stimulation for Alternative Location of Spinal Cord Stimulation in Intractable Phantom Limb Pain Syndrome: A Case Report