Ann Surg Treat Res.
2015 Dec;89(6):330-333. 10.4174/astr.2015.89.6.330.
Result of using a biologic collagen implant (Permacol) for mesenteric defect repair after excision of a huge mesenteric lymphangioma in a child
- Affiliations
-
- 1Department of Pediatric Surgery, Pusan National University Yangsan Hospital, Yangsan, Korea.
- 2Department of Pediatric Surgery, Seoul National University Children's Hospital, Seoul, Korea. spkhy02@snu.ac.kr
- KMID: 2148309
- DOI: http://doi.org/10.4174/astr.2015.89.6.330
Abstract
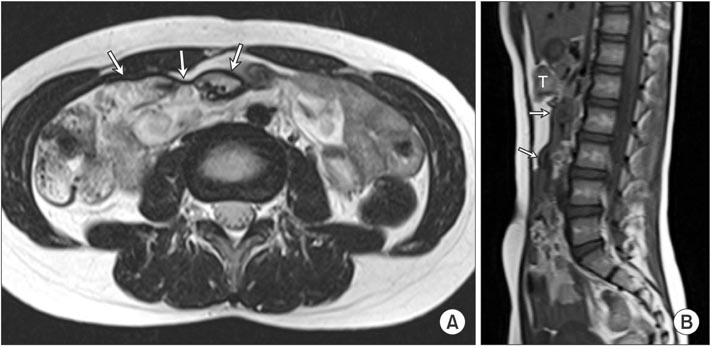
- Mesenteric lymphangiomas, which involve near total mesentery, are extremely rare. A mesenteric lymphangioma should be treated through excision because they can cause invasion of vital structures, bleeding, or infection. After excision of a huge mesenteric lymphangioma, internal herniation may occur through a large mesenteric defect leading to intestinal volvulus, obstruction, and other life-threatening circumstances. We report a case in which a biologic collagen implant (Permacol) was used for mesenteric defect repair after excision of a huge mesenteric lymphangioma. The implant did not cause any symptoms or complications during follow-up for 4 years. When encountering large defects of mesentery, closure with implant can be a feasible choice, and Permacol could be a possible implant for closing the defect.
Keyword
MeSH Terms
Figure
Reference
-
1. Okazaki T, Iwatani S, Yanai T, Kobayashi H, Kato Y, Marusasa T, et al. Treatment of lymphangioma in children: our experience of 128 cases. J Pediatr Surg. 2007; 42:386–389.2. Caro PA, Mahboubi S, Faerber EN. Computed tomography in the diagnosis of lymphangiomas in infants and children. Clin Imaging. 1991; 15:41–46.3. Losanoff JE, Richman BW, El-Sherif A, Rider KD, Jones JW. Mesenteric cystic lymphangioma. J Am Coll Surg. 2003; 196:598–603.4. Takiff H, Calabria R, Yin L, Stabile BE. Mesenteric cysts and intra-abdominal cystic lymphangiomas. Arch Surg. 1985; 120:1266–1269.5. Black PR, Mueller D, Crow J, Morris RC, Husain AN. Mesenteric defects as a cause of intestinal volvulus without malrotation and as the possible primary etiology of intestinal atresia. J Pediatr Surg. 1994; 29:1339–1343.6. de la Cruz-Munoz N, Cabrera JC, Cuesta M, Hartnett S, Rojas R. Closure of mesenteric defect can lead to decrease in internal hernias after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2011; 7:176–180.7. Cabot JC, Lee SA, Yoo J, Nasar A, Whelan RL, Feingold DL. Long-term consequences of not closing the mesenteric defect after laparoscopic right colectomy. Dis Colon Rectum. 2010; 53:289–292.8. Zheng F, Lin Y, Verbeken E, Claerhout F, Fastrez M, De Ridder D, et al. Host response after reconstruction of abdominal wall defects with porcine dermal collagen in a rat model. Am J Obstet Gynecol. 2004; 191:1961–1970.9. Kaleya RN. Evaluation of implant/host tissue interactions following intraperitoneal implantation of porcine dermal collagen prosthesis in the rat. Hernia. 2005; 9:269–276.10. Pomahac B, Aflaki P. Use of a non-crosslinked porcine dermal scaffold in abdominal wall reconstruction. Am J Surg. 2010; 199:22–27.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case Report of Chylous Mesenteric Cyst
- Experience with Porcine Acellular Dermal Collagen (Permacol(R)) Implant in Contaminated Fascia Defects
- Mesenteric and Omental Cysts in Infancy and Childhood
- A Case of Intestinal Abnormal Rotation by Mesenteric Lymphangioma
- A Mesenteric Lymphangioma Causing Billous Vomiting and Bloody Stool in a 3-day-old Infant