Ann Rehabil Med.
2015 Aug;39(4):640-644. 10.5535/arm.2015.39.4.640.
Terson Syndrome in Aneurysmal Subarachnoid Hemorrhage: A Case Report
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Research Institute of Clinical Medicine of Chonbuk National University-Biomedical Research Institute of Chonbuk National University Hospital, Jeonju, Korea. mhko@jbnu.ac.kr
- KMID: 2148237
- DOI: http://doi.org/10.5535/arm.2015.39.4.640
Abstract
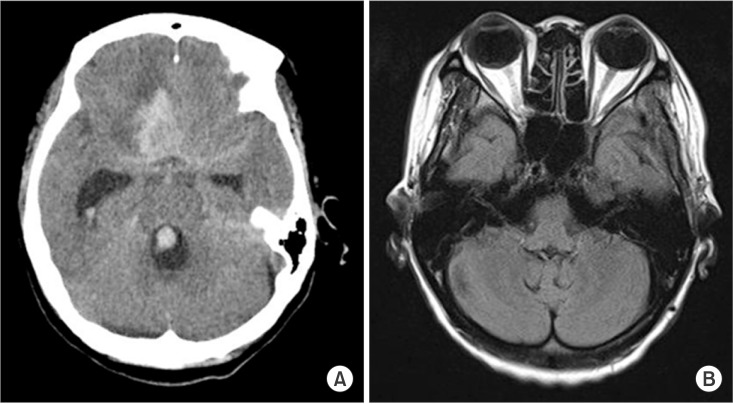
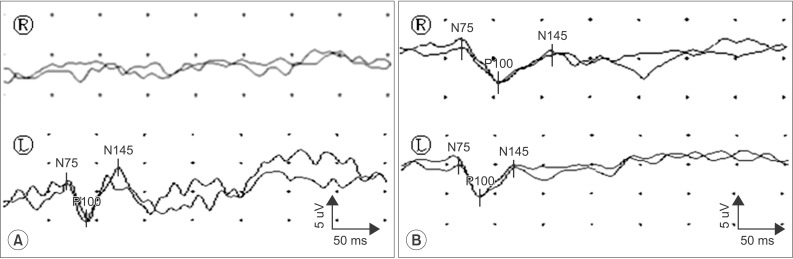
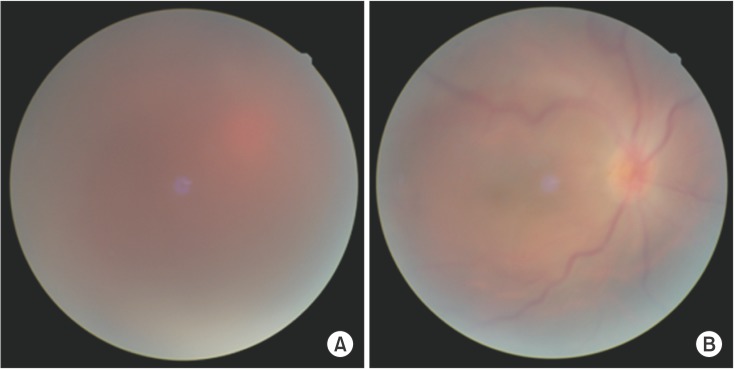
- Terson syndrome refers to oculocerebral syndrome of retinal and vitreous hemorrhage associated with spontaneous subarachnoid hemorrhage or all forms of intracranial bleeding. Recent observations have indicated that patients with spontaneous subarachnoid hemorrhage have an 18% to 20% concurrent incidence of retinal and vitreous hemorrhages with about 4% incidence of vitreous hemorrhage alone. Clinical ophthalmologic findings may have significant diagnostic and prognostic value for clinicians. Here we report a 45-year-old female patient who suffered from blurred vision after subarachnoid hemorrhage. She was diagnosed as Terson syndrome. After vitrectomy, she recovered with normal visual acuity which facilitated the rehabilitative process. We also performed visual evoked potentials to investigate abnormalities of visual dysfunction. Based on this case, we emphasize the importance of early diagnosis of Terson syndrome.
MeSH Terms
Figure
Reference
-
1. Kim US, Yu SY, Kwak HW. Incidence and postoperative visual outcome of Terson's syndrome. J Korean Ophthalmol Soc. 2002; 43:2451–2456.2. Timberlake WH, Kubik CS. Follow-up report with clinical and anatomical notes on 280 patients with subarachnoid hemorrhage. Trans Am Neurol Assoc. 1952; 56:26–30. PMID: 13038783.3. Shaw HE Jr, Landers MB, Sydnor CF. The significance of intraocular hemorrhages due to subarachnoid hemorrhage. Ann Ophthalmol. 1977; 9:1403–1405.4. Frizzell RT, Kuhn F, Morris R, Quinn C, Fisher WS 3rd. Screening for ocular hemorrhages in patients with ruptured cerebral aneurysms: a prospective study of 99 patients. Neurosurgery. 1997; 41:529–533. PMID: 9310968.
Article5. Swallow CE, Tsuruda JS, Digre KB, Glaser MJ, Davidson HC, Harnsberger HR. Terson syndrome: CT evaluation in 12 patients. AJNR Am J Neuroradiol. 1998; 19:743–747. PMID: 9576666.6. Wiethölter S, Steube D, Stotz HP. Terson syndrome: a frequently missed ophthalmologic complication in subarachnoid hemorrhage. Zentralbl Neurochir. 1998; 59:166–170. PMID: 9816667.7. Chiappa KH. Principle of evoked potentials. In : Chiappa KH, editor. Evoked potentials in clinical medicine. 3rd ed. Philadelphia: Lippincott-Raven;1977. p. 1–30.8. Wade DT, Skilbeck CE, Hewer RL. Predicting Barthel ADL score at 6 months after an acute stroke. Arch Phys Med Rehabil. 1983; 64:24–28. PMID: 6849630.9. Middleton K, Esselman P, Lim PC. Terson syndrome: an underrecognized cause of reversible vision loss in patients with subarachnoid hemorrhage. Am J Phys Med Rehabil. 2012; 91:271–274. PMID: 22019969.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Terson's Syndrome due to Subarachnoid Hemorrhage after Rupture of MCA Bifurcation Aneurysm
- Terson's Syndrome in Aneurysmal Subarachnoid Hemorrhage
- Practical Incidence and Risk Factors of Terson's Syndrome: A Retrospective Analysis in 322 Consecutive Patients with Aneurysmal Subarachnoid Hemorrhage
- Incidence and Postoperative Visual Outcome of Terson's Syndrome
- Terson Syndrome after Subarachnoid Hemorrhage Occurred by Thrombolysis and Mechanical Thrombectomy to Treat Acute Ischemic Stroke: A Case Report