Korean Circ J.
2010 Apr;40(4):191-196. 10.4070/kcj.2010.40.4.191.
Morphologic Characteristics and Relating Factors to the Need of Technical Modification in Transcatheter Closure of Large Atrial Septal Defect (> or =25 mm)
- Affiliations
-
- 1Division of Pediatric Cardiology, Severance Cardiovascular Hospital, Yonsei University Health System, Seoul, Korea. cjy0122@yuhs.ac
- KMID: 2145556
- DOI: http://doi.org/10.4070/kcj.2010.40.4.191
Abstract
- BACKGROUND AND OBJECTIVES
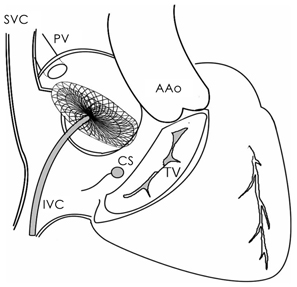
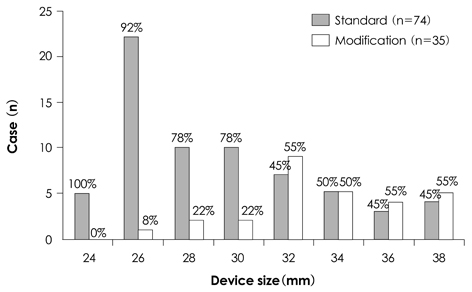
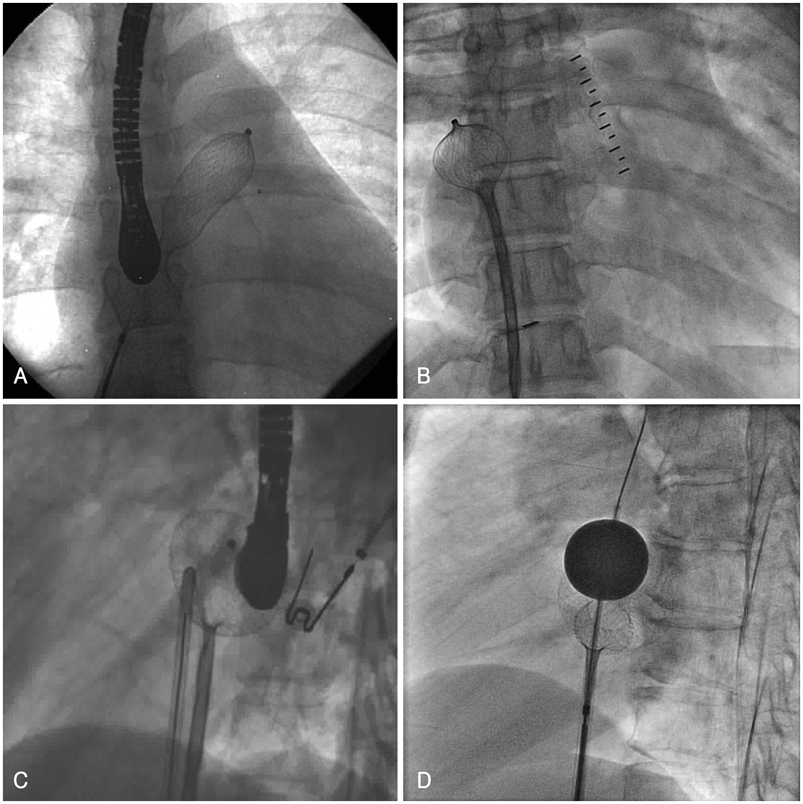
The rigid coupling between the delivery wire and the right atrial disk has been occasionally encountered during transcatheter closure of atrial septal defect (ASD). Therefore the device frequently makes a perpendicular angle, and the leading edge of left atrial disk slips through the defect and prolapses into right atrium (RA) before it is properly placed in the septum. The purpose of this study is to investigate relating factors to the need of technical modification in transcatheter closure of large ASD and to evaluate relevant morphologic characteristics of atrial septal rim in this situation. SUBJECTS AND METHODS: From July, 2003 to May, 2007, 312 patients underwent transcatheter occlusion of ASD with Amplatzer Septal Occluder(R) (ASO, AGA medical corporation, Golden Valley, MN, USA) at Yonsei Cardiovascular Center and among them 109 patients had large ASD (> or =25 mm) and these patients were enrolled in our study. Patients were divided into two groups according to the deploying methods of the device (Group I: standard method, Group II: modified methods). Assessments of the defects and its surrounding rims were made by echocardiography. RESULTS: There were no differences between 2 groups in age, body weight and height except for balloon-stretched diameter (stop-flow technique) and device size. Group II patients with modified methods showed larger balloon-stretched diameter and device size than group I patients with standard method. The mean length of anterosuperior (AS) rim in group II was significantly shorter than group I (p<0.05). As the size of the device used in procedure increased, there was a trend towards increase in the need of modified methods. CONCLUSION: This study shows that AS rim deficiency and the size of ASD may be the relating factors to the need of technical modification in transcatheter closure of ASD. Therefore, when the initial try with standard method is not successful in large ASD with deficient AS rim, we suggest that changing strategy of implantation may save time and efforts and possibly reduce the risk of complications associated with prolonged procedure.
MeSH Terms
Figure
Reference
-
1. Rao PS. Catheter closure of atrial septal defects. J Invasive Cardiol. 2003. 15:398–400.2. Ebeid MR. Percutaneous catheter closure of secundum atrial septal defects: a review. J Invasive Cardiol. 2002. 14:25–31.3. Berger F, Vogel M, Alexi-Meskishvili V, Lange PE. Comparison of results and complications of surgical and Amplatzer device closure of atrial septal defects. J Thorac Cardiovasc Surg. 1999. 118:674–678. discussion 678-80.4. Chessa M, Carminati M, Butera G, et al. Early and late complications associated with transcatheter occlusion of secundum atrial septal defect. J Am Coll Cardiol. 2002. 39:1061–1065.5. Du ZD, Hijazi ZM, Kleinman CS, Silverman NH, Larntz K. Comparison between transcatheter and surgical closure of secundum atrial septal defect in children and adults: results of a multicenter nonrandomized trial. J Am Coll Cardiol. 2002. 39:1836–1844.6. Spies C, Hijazi ZM. Transcatheter closure of secundum atrial septal defects in the elderly. Korean Circ J. 2009. 39:47–51.7. Varma C, Benson LN, Silversides C, et al. Outcomes and alternative techniques for device closure of the large secundum atrial septal defect. Catheter Cardiovasc Interv. 2004. 61:131–139.8. Aeschbacher BC, Chatterjee T, Meier B. Transesophageal echocardiography to evaluate success of transcatheter closure of large secundum atrial septal defects in adults using the buttoned device. Mayo Clin Proc. 2000. 75:913–920.9. Berger F, Ewert P, Dhnert I, et al. Interventional occlusion of atrial septum defects larter than 20 mm in diameter. Z Kardiol. 2000. 89:1119–1125.10. Dalvi BV, Pinto RJ, Gupta A. New technique for device closure of large atrial septal defects. Catheter Cardiovasc Interv. 2005. 64:102–107.11. Fu YC, Cao QL, Hijazi ZM. Device closure of large atrial septal defects: technical considerations. J Cardiovasc Med (Hagerstown). 2007. 8:30–33.12. Kutty S, Asnes JD, Srinath G, Preminger TJ, Prieto LR, Latson LA. Use of a straight, side-hole delivery sheath for improved delivery of Amplatzer ASD occluder. Catheter Cardiovasc Interv. 2007. 69:15–20.13. Staniloae CS, El-Khally Z, Ibrahim R, Dore A, De Guise P, Mercier LA. Percutaneous closure of secundum atrial septal defect in adults a single center experience with the Amplatzer septal occluder. J Invasive Cardiol. 2003. 15:393–397.14. Zhu W, Cao QL, Rhodes J, Hijazi ZM. Measurement of atrial septal defect size: a comparative study between three-dimensional transesophageal echocardiography and the standard balloon sizing methods. Pediatr Cardiol. 2000. 21:465–469.15. Douglas PS, DeCara JM, Devereux RB, et al. Echocardiographic imaging in clinical trials: American Society of Echocardiography Standards for echocardiography core laboratories: endorsed by the American College of Cardiology Foundation. J Am Soc Echocardiogr. 2009. 22:755–765.16. Wahab HA, Bairam AR, Cao Q, Hijazi ZM. Novel technique to prevent prolapse of the Amplatzer septal occluder through large atrial septal defect. Catheter Cardiovasc Interv. 2003. 60:543–545.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transcatheter Closure of Atrial Septal Defect: Does Age Matter?
- Procedural, Early and Long-Term Outcomes after Transcatheter Atrial Septal Defects Closure: Comparison between Large and Very Large Atrial Septal Defect Groups
- Comprehensive understanding of atrial septal defects by imaging studies for successful transcatheter closure
- Outcome of Transcatheter Closure of Oval Shaped Atrial Septal Defect with Amplatzer Septal Occluder
- Emergent Surgical Intervention for Embolization of Atrial Septal Defect Closure Device