Korean J Urol.
2006 Dec;47(12):1302-1308. 10.4111/kju.2006.47.12.1302.
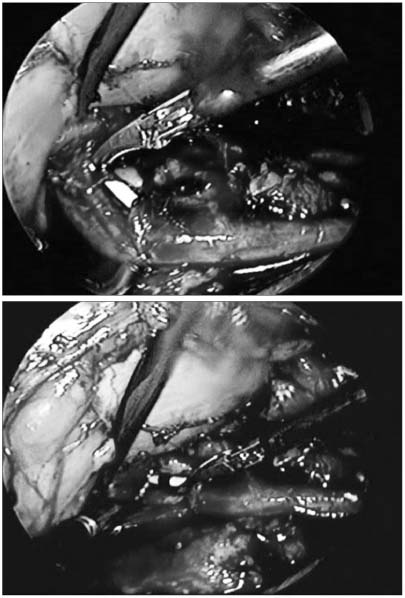
Initial Experience of Laparoscopic Pyeloplasty: Retrograde Stenting Using Flexible Cystoscopes
- Affiliations
-
- 1Department of Urology, Eulji University, Daejeon, Korea. sblee@eulji.ac.kr
- 2Department of Diagnostic Radiology, Eulji University, Daejeon, Korea.
- KMID: 2139775
- DOI: http://doi.org/10.4111/kju.2006.47.12.1302
Abstract
- PURPOSE
To describe our initial experience of laparoscopic pyeloplasty, with retrograde stenting, using flexible cystoscopes, in 9 cases of ureteropelvic junction obstruction (UPJO).
MATERIALS AND METHODS
Between September, 2004 and January, 2006, 9 cases of UPJO were treated by laparoscopic pyeloplasty. All of the medical records were reviewed retrospectively. The cases comprised of 5 males and 4 females, with a mean age of 37 years (13-58). All patients showed a preoperative grade 4 hydronephrosis.
RESULTS
Two laparoscopic pyeloplasty approaches were performed; a transperitoneal approach in 5 cases and a retroperitoneal approach in the other 4. All cases were treated with dismembered Anderson-Hynes pyeloplasty. The mean operating time was 249 minutes (170-324), including a mean of 7.1 minutes (6.5-8) for ureteral stenting. The patients were found to have aberrant vessels and renal stones in 1 and 3 cases, respectively. There were no intra-operative complications or open conversion. Of the 9 cases, 8 (89%) showed a decrease in their hydronephrosis grade on the excretory urographs taken 12 weeks postoperatively. The remaining case showed a marked improvement in the hydronephrosis, despite having no change in the hydronephrosis grade. No case experienced postoperative flank pain or recurrence of acute pyelonephritis. Therefore, symptomatic improvements were observed in all our cases (100%).
CONCLUSIONS
Laparoscopic pyeloplasty, with retrograde stenting, using flexible cystoscopes, can be considered an effective and convenient method for the treatment of UPJO.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Experience with Laparoscopic Pyeloplasty, Including Robot-Assisted Laparoscopic Surgery, for Ureteropelvic Junction Obstruction
Seong Cheol Kim, Taejin Kang, Hyungkeun Park
Korean J Urol. 2009;50(10):996-1002. doi: 10.4111/kju.2009.50.10.996.
Reference
-
1. Lowe FC, Marschall FF. Ureteropelvic junction obstruction in adults. Urology. 1984. 23:331–335.2. O'Reilly PH, Brooman PJ, Mak S, Jones M, Pickup C, Atkinson C, et al. The long-term results of Anderson-Hynes pyeloplasty. BJU Int. 2001. 87:287–289.3. Schuessler WW, Grune MT, Tecuanhuey LV, Preminger GM. Laparoscopic dismembered pyeloplasty. J Urol. 1993. 150:1795–1799.4. Kavoussi LR, Peters CA. Laparoscopic pyeloplasty. J Urol. 1993. 150:1891–1894.5. Streem SB, Franke JJ, Smith JA Jr. Walsh PC, Retik AB, Vaughan ED, Wein AJ, editors. Management of upper urinary tract obstruction. Campbell's urology. 2002. 8th ed. Philadelphia: Saunders;487–489.6. Hwangbo K, Seo SI, Kim JC, Hwang TK. Retroperitoneoscopic pyeloplasty. Korean J Urol. 2003. 44:624–627.7. Seo IY, Park SC, Oh SJ. Laparoscopic pyeloplasty with transperitoneal approach for ureteropelvic obstruction. Korean J Urol. 2005. 46:370–374.8. Talner LB, O'Reilly PH, Roy C. Pollack HM, McClennan BL, Dyer R, Kenney PJ, editors. Urinary obstruction. Clinical urography. 2000. 2nd ed. Philadelphia: Saunders;1846–1966.9. Brooks JD, Kavoussi LR, Preminger GM, Schuessler WW, Moore RG. Comparison of open and endourologic approaches to the obstructed ureteropelvic junction. Urology. 1995. 46:791–795.10. Van Cangh PJ, Jorion JL, Wese FX, Opsomer RJ. Endoureteropyelotomy: percutaneous treatment of ureteropelvic junction obstruction. J Urol. 1989. 141:1317–1321.11. Van Cangh PJ, Wilmart JF, Opsomer RJ, Abi-Aad A, Wese FX, Lorge F. Long-term results and late recurrence after endoureteropyelotomy: a critical analysis of prognostic factors. J Urol. 1994. 151:934–937.12. Motola JA, Badlani GH, Smith AD. Results of 212 consecutive endopyelotomies: an 8-year followup. J Urol. 1993. 149:453–456.13. Tan BJ, Smith AD. Ureteropelvic junction obstruction repair: when, how, what? Curr Opin Urol. 2004. 14:55–59.14. Jarrett TW, Chan DY, Charambura TC, Fugita O, Kavoussi LR. Laparoscopic pyeloplasty: the first 100 cases. J Urol. 2002. 167:1253–1256.15. Zhang X, Li HZ, Wang SG, Ma X, Zheng T, Fu B, et al. Retroperitoneal laparoscopic dismembered pyeloplasty: experience with 50 cases. Urology. 2005. 66:514–517.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Outcome of Tubeless Dismembered Pyeloplasty in Adult Ureteropelvic Junction Obstruction and Significance of Double-J Ureteral Stenting
- The Experience of Modified Flexible Cystoscopy in Male Patients
- Experience with Laparoscopic Pyeloplasty, Including Robot-Assisted Laparoscopic Surgery, for Ureteropelvic Junction Obstruction
- Laparoscopic Pyeloplasty with Transperitoneal Approach for Ureteropelvic Obstruction
- Initial Experience of Flexible Cystourethroscope