J Korean Med Assoc.
2007 Feb;50(2):127-133. 10.5124/jkma.2007.50.2.127.
Assessment of Coronary Artery Bypass Graft Patency Using Multidetector Computed Tomography
- Affiliations
-
- 1Department of Radiology, University of Ulsan College of Medicine, Korea. seojb@amc.seoul.kr
- KMID: 2137785
- DOI: http://doi.org/10.5124/jkma.2007.50.2.127
Abstract
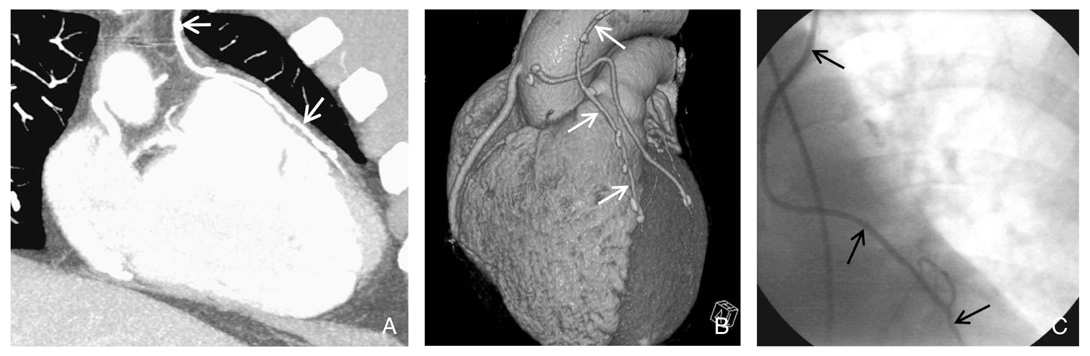
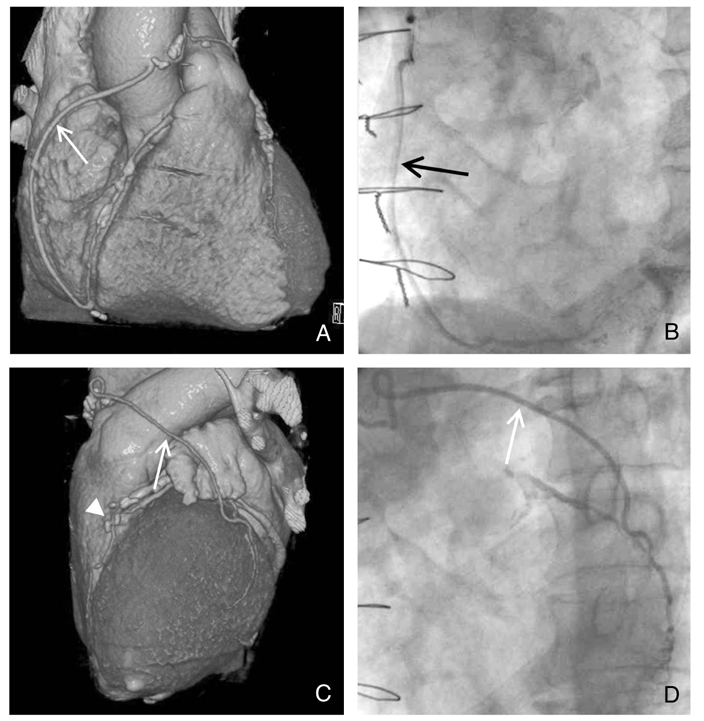
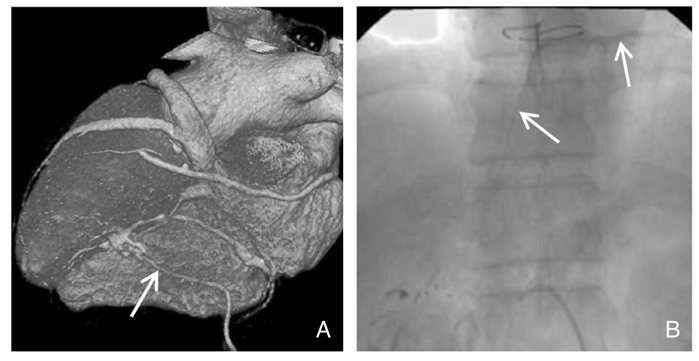
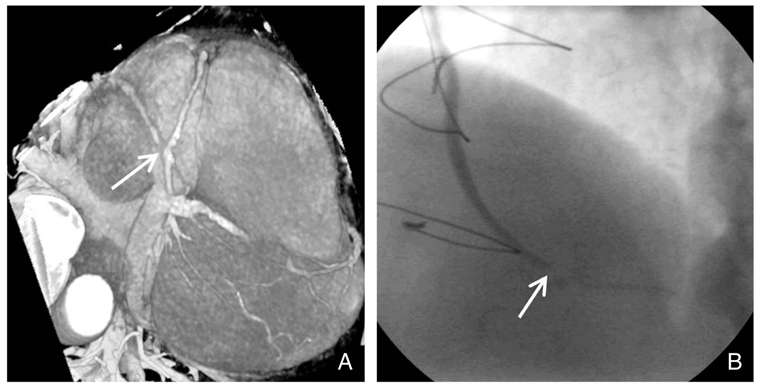
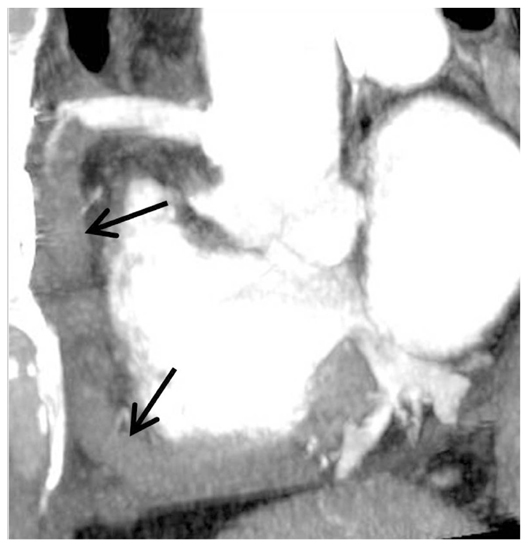
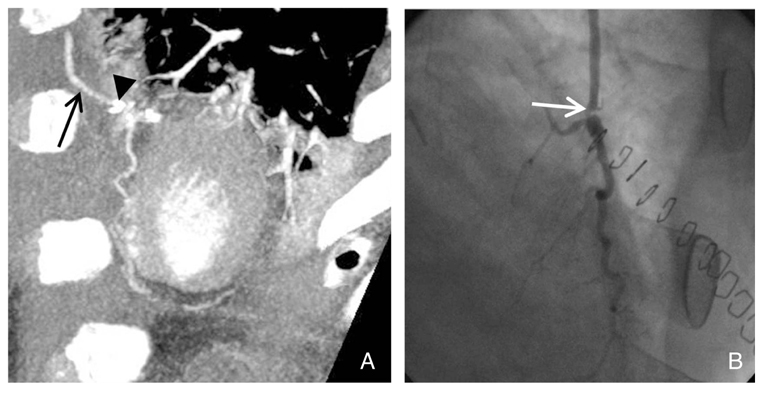
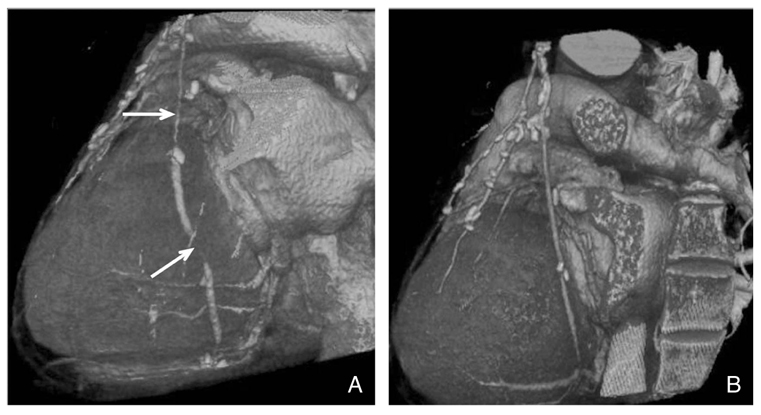
- Coronary artery bypass graft surgery (CABG) is the standard of care in the treatment of advanced coronary artery disease. Invasive coronary angiography has been used to assess the status of graft. Recently, multidetector computed tomography (MDCT) has emerged as an important diagnostic tool for the evaluation of graft patency. Many studies have shown that MDCT has a high sensitivity and specificity in detecting graft occlusion or high-grade stenosis. However, there are several diagnostic pitfalls in evaluating CABG graft patency due to several factors, including technical factors, patient factors, and flow competition. Acknowledgment of these pitfalls and remedies to avoid wrong interpretation is essential to improve diagnostic accuracy. In addition, MDCT yields additional information such as plural effusion, pericardial effusion, sternal infection, pneumonia, pulmonary embolism, and so on. The continuing advance in the MDCT technology suggests that MDCT will be a rapid, convenient, and noninvasive tool in evaluating CABG patients in the near future.
MeSH Terms
Figure
Reference
-
1. Bourassa MG, Fisher LD, Campeau L, Gillespie MJ, Mc-Conney M, Lesperance J. Long-term fate of bypass grafts: the coronary artery surgery study (CASS) and Montreal Heart Institute experiences. Circulation. 1985. 72:V71–V78.2. Aruny JE. Baum S, editor. Complications of coronary arteriography. Abrams' angiography: vascular and interventional radiology. 1997. 4th ed. Boston: Little, Brown and Company;572–582.3. de Bono DP, Samani NJ, Spyt TJ, Hartshorne T, Thrush AJ, Evans DH. Transcutaneous ultrasound measurement of blood-flow in internal mammary artery to coronary artery grafts. Lancet. 1992. 339:379–381.
Article4. Gomes AS, Lois JF, Drinkwater DC Jr, Corday SR. Coronary artery bypass grafts: visualization with MR imaging. Radiology. 1987. 162:175–179.
Article5. Langerak SE, Vliegen HW, de Roos A, Zwinderman AH, Jukema JW, Kunz P, Lamb HJ, van Der Wall EE. Detection of vein graft disease using high-resolution magnetic resonance angiography. Circulation. 2002. 105:328–333.
Article6. Ha JW, Cho SY, Shim WH, Chung N, Jang Y, Lee HM, Choe KO, Chung WJ, Choi SH, Yoo KJ, Kang MS. Noninvasive evaluation of coronary artery bypass graft patency using three-dimensional angiography obtained with contrast-enhanced electron beam CT. Am J Roentgenol. 1999. 172:1055–1059.
Article7. Achenbach S, Moshage W, Ropers D, Nossen J, Bachmann K. Noninvasive, three-dimensional visualization of coronary artery bypass grafts by electron beam tomography. Am J Cardiol. 1997. 79:856–861.
Article8. Ueyama K, Ohashi H, Tsutsumi Y, Kawai T, Ueda T, Ohnaka M. Evaluation of coronary artery bypass grafts using helical scan computed tomography. Catheter Cardiovasc Interv. 1999. 46:322–326.
Article9. Hong C, Becker CR, Huber A, Schoepf UJ, Ohnesorge B, Knez A, Bruning R, Reiser MF. ECG-gated reconstructed multi-detector row CT coronary angiography: effect of varying trigger delay on image quality. Radiology. 2001. 220:712–717.
Article10. Kim HJ, Seo JB, Lee YK, Do KH, Heo JN, et al. ECG-gated CT angiography for the assessment of coronary bypass graft patency: the influence of heart rate, type of bypass graft, target vessel and surgical technique on the diagnostic accuracy. J Korean Radiol Soc. 2006. 54:11–17.
Article11. Ropers D, Ulzheimer S, Wenkel E, Baum U, Giesler T, Derlien H, Moshage W, Bautz WA, Daniel WG, Kalender WA, Achenbach S. Investigation of aortocoronary artery bypass grafts by multislice spiral computed tomography with electrocardiographic-gated image reconstruction. Am J Cardiol. 2001. 88:792–795.
Article12. Nieman K, Pattynama PMT, Rensing BJ, van Geuns R-JM, de Feyter PJ. Evaluation of patients after coronary artery bypass surgery: CT angiographic assessment of grafts and coronary arteries. Radiology. 2003. 229:749–756.
Article13. Marano R, Storto ML, Maddestra N, Bonomo L. Non-invasive assessment of coronary artery bypass graft with retrospectively ECG-gated four-row multi-detector spiral computed tomography. Eur Radiol. 2004. 14:1353–1362.
Article14. Schlosser T, Konorza T, Hunold P, Kuhl H, Schmermund A, Barkhausen J. Noninvasive visualization of coronary artery bypass grafts using 16-detector row computed tomography. J Am Coll Cardiol. 2004. 44:1224–1229.
Article15. Ropers D, Pohle FK, Kuettner A, Pflederer T, Anders K, Daniel WG, Bautz W, Baum U, Achenbach S. Diagnostic accuracy of noninvasive coronary angiography in patients after bypass surgery using 64-slice spiral computed tomography with 330-ms gantry rotation. Circulation. 2006. 114:2334–2341.
Article16. Frazier AA, Qureshi F, Read KM, Gilkeson RC, Poston RS, White CS. Coronary artery bypass grafts: assessment with multidector CT in the early and late postoperative settings. RadioGraphics. 2005. 25:881–896.
Article17. Rossi R, Chiurlia E, Ratti C, Ligabue G, Romagnoli R, Modena MG. Noninvasive assessment of coronary artery bypass graft patency by multislice computed tomography. Ital Heart J. 2004. 5:36–41.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Multidetector Computed Tomography with Coronary Angiography for Evaluation of Coronary Artery Bypass Grafts
- Assessment of Coronary Artery Bypass Graft Patency Using Three Dimensional Coronary Angiography by Electron Beam Tomography
- Determination of Early Graft Patency Using CT Angiography after Coronary Artery Bypass Surgery
- The Noninvasive Diagnosis and Postoperative Evaluation of Anomalous Right Coronary Artery from the Pulmonary Artery (ARCAPA) using Coronary MDCT: A Case Report
- The Right Gastroepiploic Artery Graft for Coronary Artery Bypass Grafting: A 30-Year Experience